The discomfort consists of a persistent burning and soreness in the genital area. Tight pants are uncomfortable, sitting and riding a bicycle become difficult, and intercourse is almost unthinkable. The affected women then visit many gynecologists. However, no organic findings are found. This symptomatology is called vulvodynia. What is it? How does it develop? What should be done?
What is vulvodynia?
Definition
Vulvodynia is described as "discomfort in the area of the vaginal entrance, usually described as a burning pain, without any relevant findings or a clear neurological disease".
For terminology: vulva = totality of the external female sexual organs i.e. mons veneris, labia majora and minora, clitoris and vaginal vestibule.
Vulvodynia is therefore a pain disorder of the vulva.
Complaints
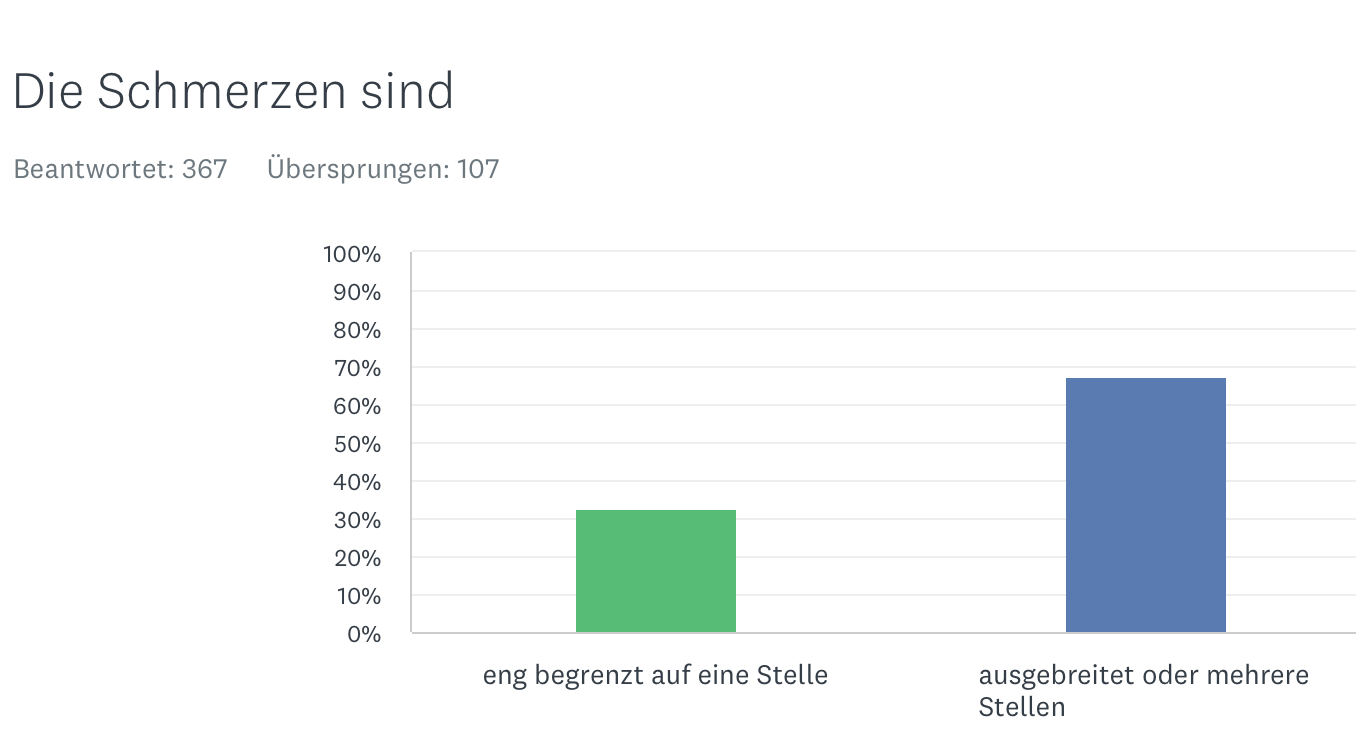
The pain varies in intensity. It can either extend diffusely to the vaginal entrance or be locally limited to a specific area of the vulva. Especially after a longer period of suffering, the complaints may also spread to the bladder (e.g. during urination) or the pelvic floor.
After a longer period of suffering, other functional complaints occur in addition to vulvodynia, not infrequently coupled with depressed mood or increased anxiety.
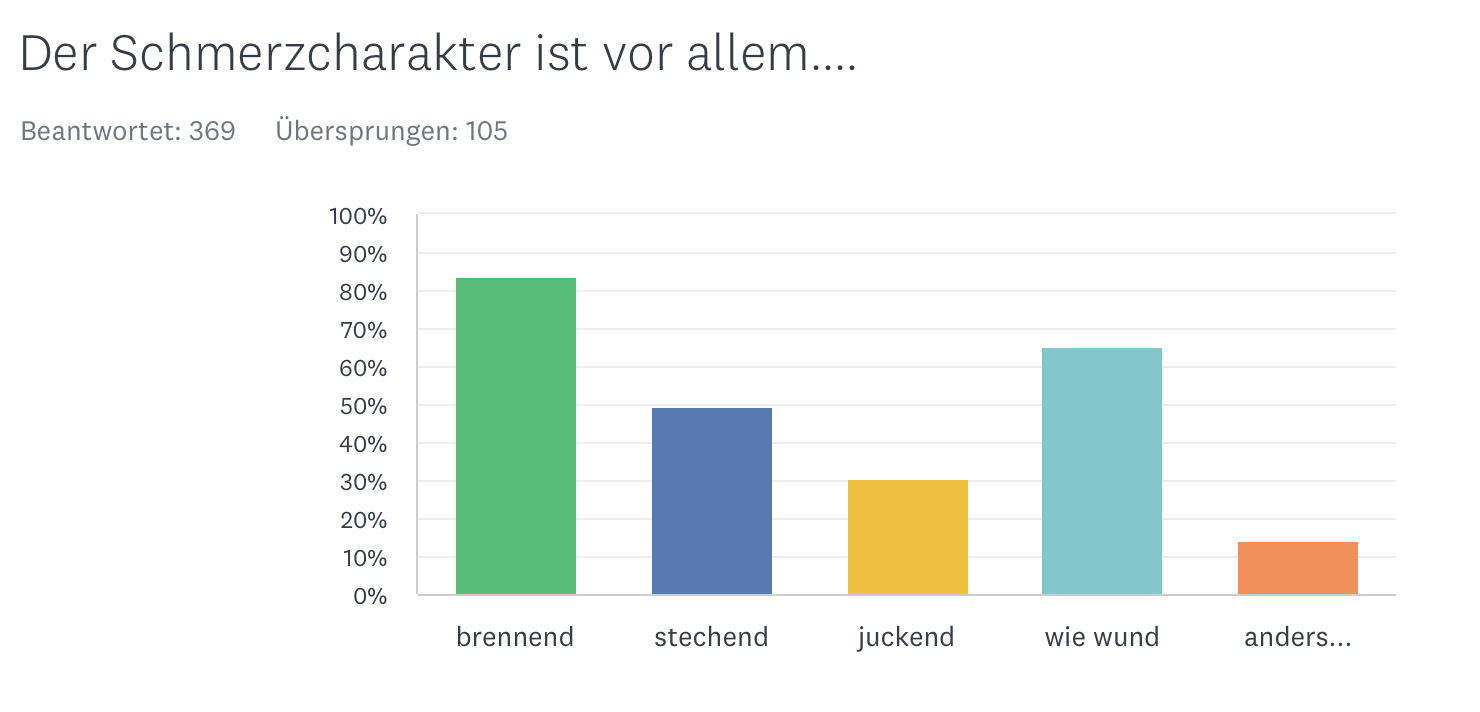
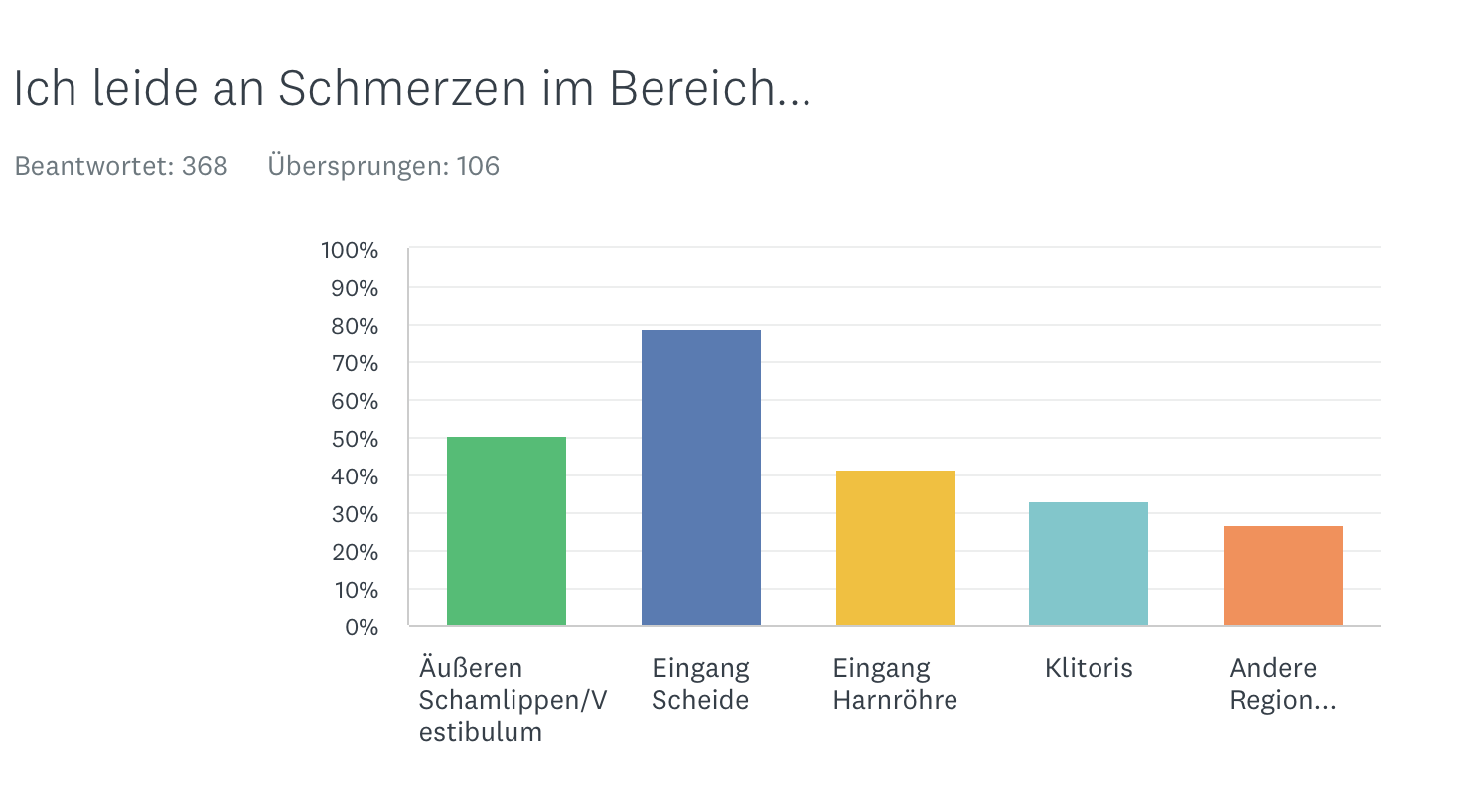
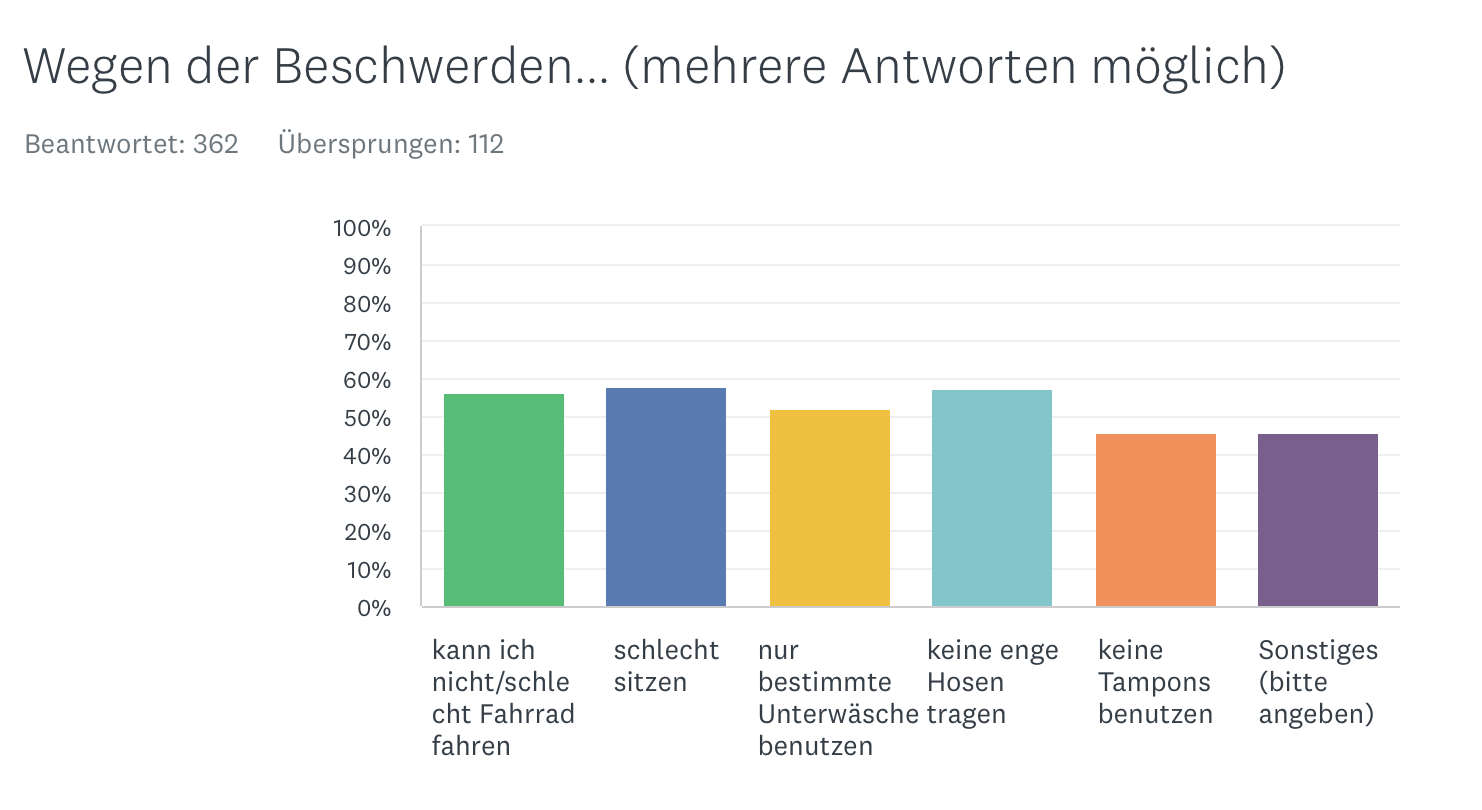
According to our own investigations, the following complaints are in the foreground:
Pain character
Pain site
Restrictions
Frequency
Vulvodynia is a surprisingly common condition. According to American studies, 3-7% of women of childbearing age suffer from the condition at least intermittently. In other studies, the number of women was even higher. In a study of 4915 women in Boston, USA, 16% reported the problem at some time in the past ("lifetime prevalence") and 7% suffered from acute symptoms.
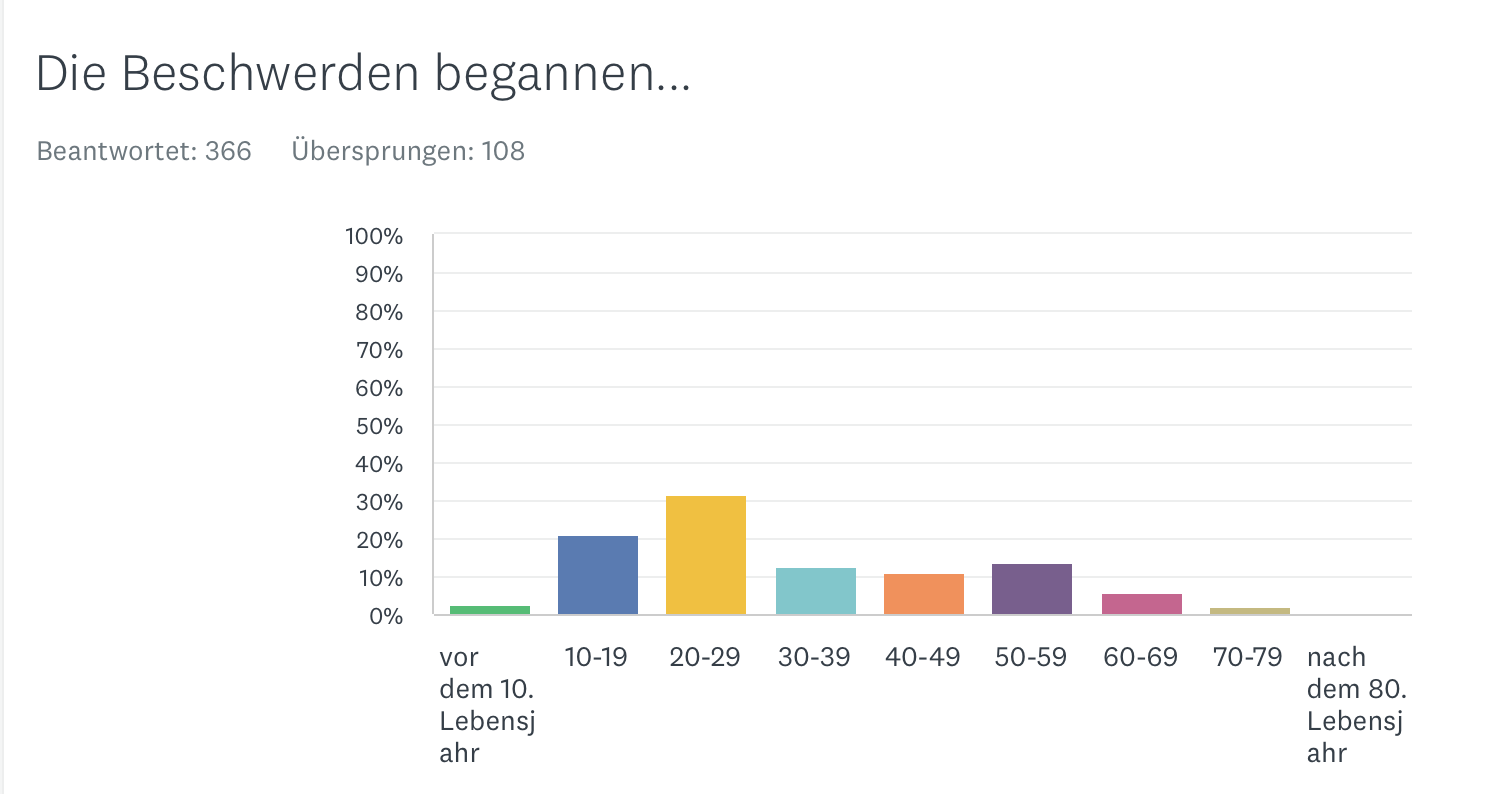
Young women between 18 to 25 years of age were reported to be most commonly affected, but ages ranged from adolescents to the very elderly. No significant difference between different cultures was found.
According to our study, there is a two-peaked distribution with a peak at a young age and one around menopause.
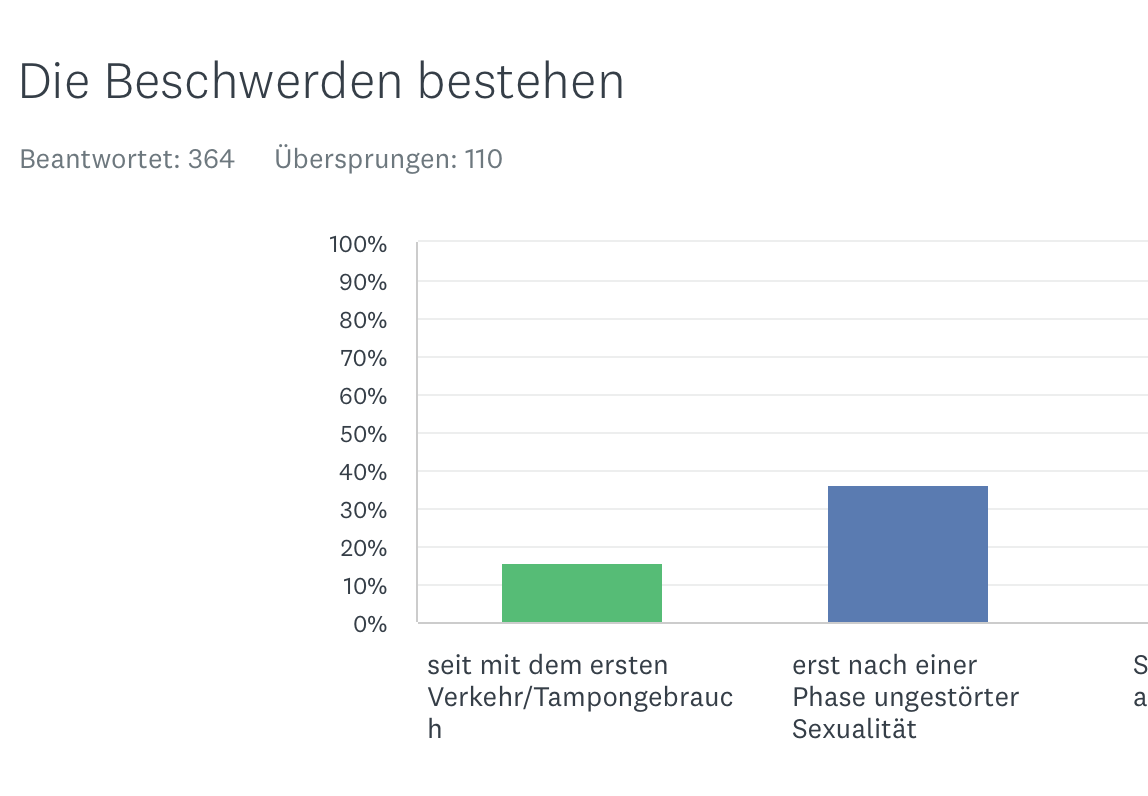
Complaint start
Forms
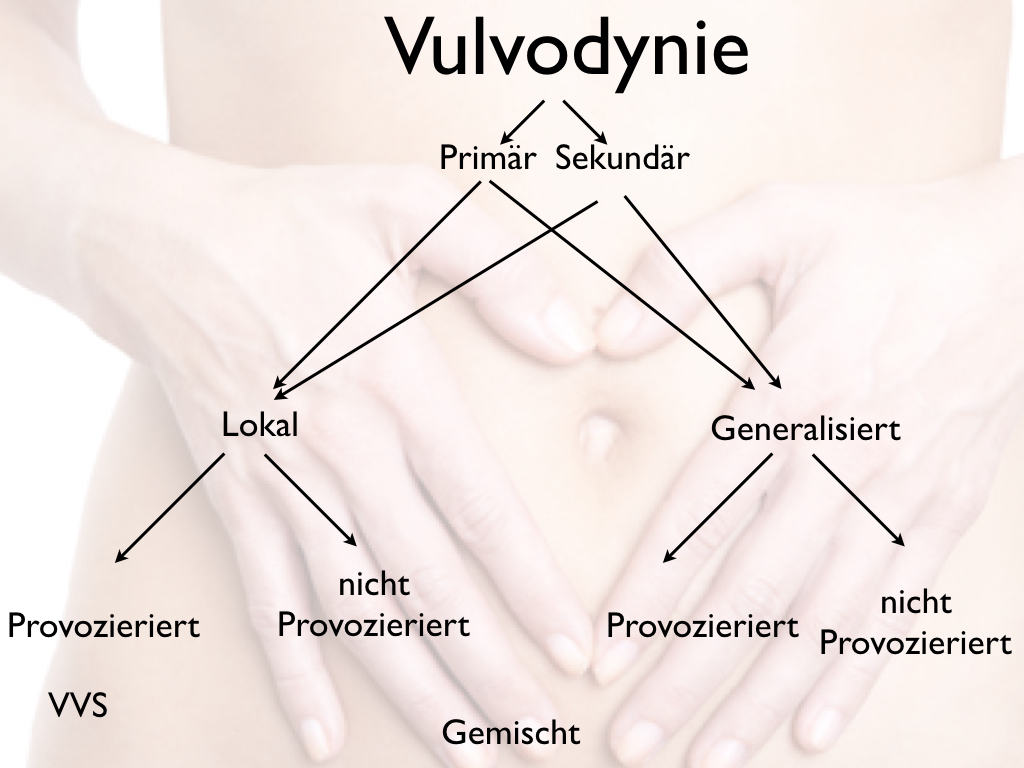
Primary vulvodynia
Occurs with first use of tampons or first intercourse
Secondary vulvodynia
After a period without symptoms
Local vulvodynia
Pain is limited to single areas. When touched (e.g., cotton swab), redness may appear. This constellation is also called VVS (vulvar vestibulitis syndrome).
Generalized vulvodynia
In this type, the entire vulva burns/pains.
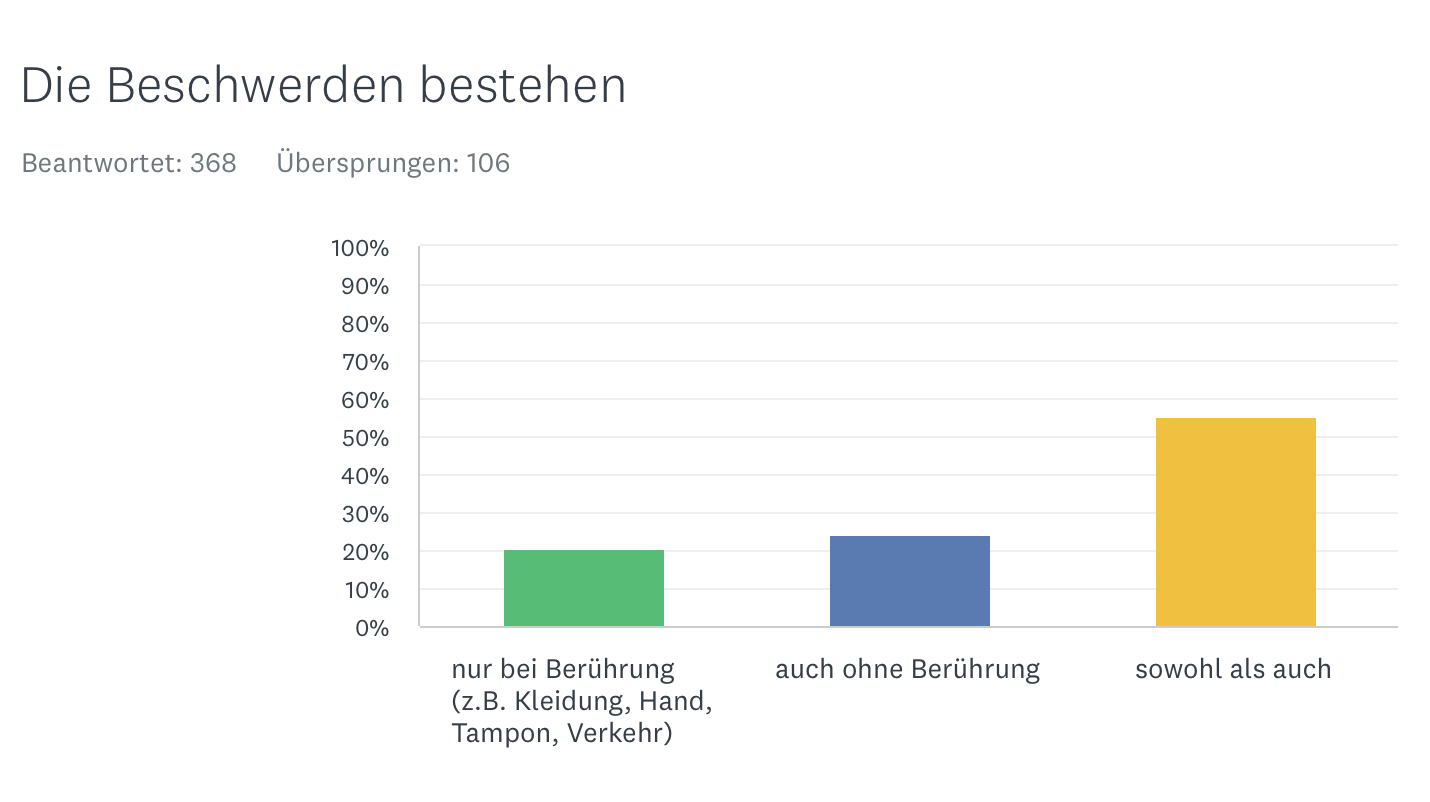
Provoked vulvodynia
In some women, the pain occurs only when there is an external stimulus, usually touch, such as during intercourse, tampon, or by tight clothing. This is called "provoked vulvodynia."
Not provoked
In contrast - and this is usually after a longer period of suffering - the pain can also occur without any external cause ("unprovoked vulvodynia"). According to our research, however, most of those affected suffer from a mixed form.
There are very different data in the literature on the frequency of occurrence.
We have conducted a large online survey. Here are the current figures.
Primary-Secondary
Localized - generalized
Provoked - not provoked
Trigger
The data and research situation on vulvodynia is still very limited despite the frequency of the complaints. Therefore, there is often a lack of clear information on the frequency, causes, etc.In the first place, infections in the genital area should be mentioned. Ultimately (especially long-lasting or painful/angry) infections are associated with a higher risk of later developing vulvodynia.
- Fungal infections (thrush)
- Bacterial infections
- Trichomonads
- Bladder infections
- Genital herpes
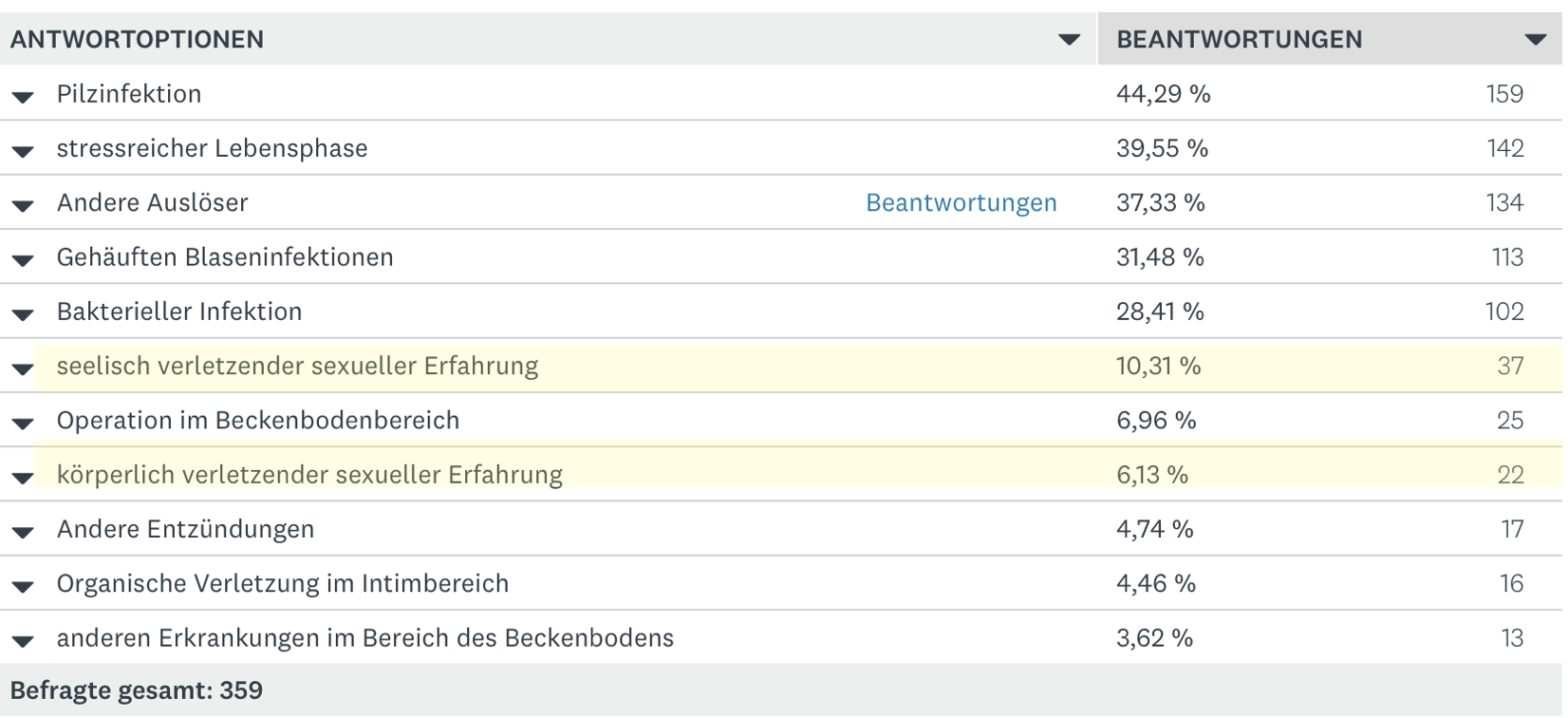
Especially the risk increases when frequent/various infections occur over a longer period of time.Here are the results of our study on vulvodynia.
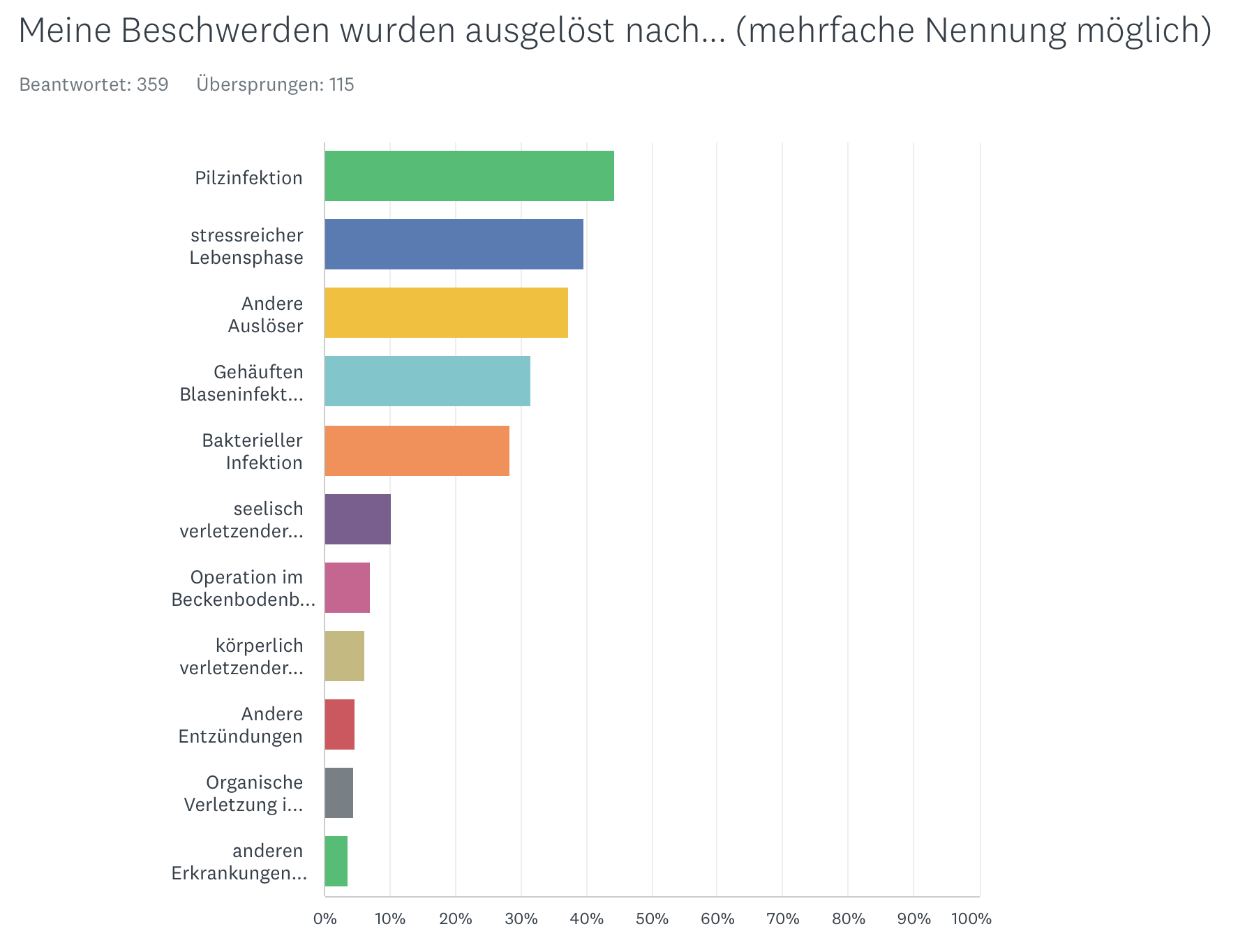
Painful sexual experiences
Although at first glance it seems very obvious that painful sexual experiences promote vulvodynia, the scientific data situation is unclear. While some of the studies affirm this, other studies cannot establish a connection between experiences of abuse and later vulvodynia.
From our own experience with female patients, these cases do occur, but they are - fortunately! - in the minority. Only 10% report emotional and 6% also physical sexual injury.
Thus, the frequent insinuation that vulvodynia is due to a (perhaps forgotten) experience of violence has no basis. Of course, this only applies to our patients. This may be different, for example, in other regions of the world or after armed conflicts.
Causes
Central sensitization
Research findings suggest that central sensitization is primarily responsible for pain. "Central sensitization" is the common cause of a variety of so-calledfunctional disorders. Therefore, these complaints often occur in combination.
Other factors
However, regional persistent pain has (measurable) consequences. This is evident in research studies. A number of elevated neurotransmitters have been found. However, these findings do not mean that this is the cause of the complaints. Among other things, the following were found
- Increased inflammatory factors (including cytokines, TNF-alpha, interleukins)
- Increased number of white blood cells (lymphocytes, leukocytes, mast cells)
- Mild inflammation of the mucosa
- At least during the course of the disease: Increased innervation in the affected tissue, i.e. increased nerve formation
- Certain gene variants (gene polymorphisms) occur more frequently in vulvodynia.
Research findings that indicate that affected individuals have increased sensitivity in other respects are also likely to be significant:
- Increased sensitivity to pressure (in the body region).
- High brain activity in pain regions (hippocampus, basal ganglia, somatosensory cortex)
- Stronger response to chemical pain stimuli (capsaicin)
- Higher sensitivity to cold
Other concomitant diseases
- Interstitial cystitis (IC)
- Irritable bladder
- Pain disorders:fibromyalgia, facial pain (temporomandibular dysfunction, atypical facial pain)
- Irritable bowel syndrome
- Sexual impairments
- Functional disorders
- Anxiety disorders, depression
- Panic disorders
Respiratory
In recent years, we have seen that in a significant number of patients - in fact, the vast majority - persistent pain leads to stress-related changes in breathing. In most cases, there is at least a mild form of chronic hyperventilation. This fact is significant in that this increases the tension in the pelvic floor and increases sensitivity.
Candida & Co
Very many female patients have a long history of fungal diseases. In our study, more than 80% used a medication at least for this reason. It is not uncommon for such complaints to occur after taking antibiotics.
It is well known - and also reproducible in animal experiments - that Candida albicans (the most common pathogen) leads to a significant irritation of the nerves in the tissue.
Subsequently, at least some of the women experience increased sensitivity to small or minute amounts of Candida. Even if germs are not detectable or only in traces, symptoms similar to those of a fungal infection of the vagina occur.
Damage due to therapy
Creams, ointment, pads can also either irritate mechanically or lead to allergic problems. Surgical interventions are particularly problematic, which then lead to wounds and thus lower the irritation threshold even further.
Many sufferers can look back on a veritable odyssey of doctors. Sometimes it is the case that the complaints get worse the more doctors are consulted. (Of course, every doctor tries to improve the symptoms to the best of his knowledge).
Therefore, over-diagnosis and over-therapy - despite all the good will of those involved - is often an additional risk factor!
In the end, some women have the impression that their whole life revolves around the constant burning. This leads to a self-reinforcement of the symptoms.
Summary
From our point of view vulvodynia belongs at least in essence to the large group of sensitization disorders. Here again the causes are summarized:
In the beginning there is a repeated external stimulus. Usually this is triggered by infections (fungi, bacteria, viruses) or a mechanical stimulus irritates the mucosa. The associated internal disturbance also plays a role. When questions arise such as "What do I have?", "Will this go away?", "Will this affect my sexuality?", "How will my partner adjust to this?" then attention is involuntarily directed to the vulva and thus - of course unconsciously - perception is intensified. To avoid any misunderstanding: The increased attention can hardly be avoided, if at all. It is hardly possible not to think about the pain/burning.
Initially, therefore, increased stimuli come from the region of the vaginal entrance. The body reacts with increased attention or stimulus swelling. After a while, the local infection subsides. But the increased sensitivity to stimuli remains.
Associated complaints
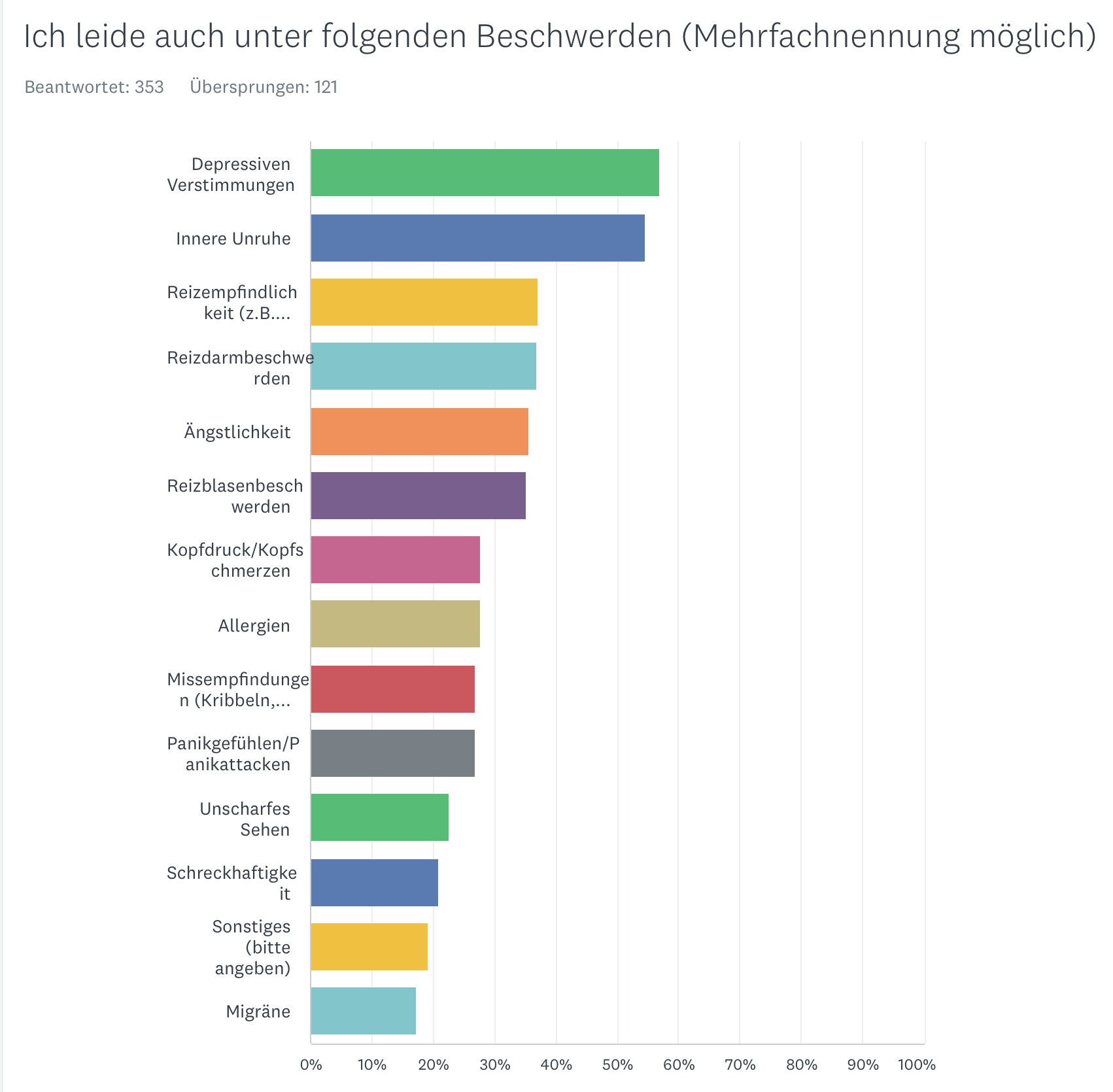
As with most vegetative complaints, vulvodynia pelvic floor pain does not occur in isolation, but is usually accompanied by other symptoms that you will find on these pages.
This may surprise you, but from our point of view it is completely logical, as we understand vulvodynia syndrome in the context of the body's emergency programs.
You will findmore details hereand also on many other pages, e.g. onfibromyalgia syndrome,irritable bowel syndrome or irritable bladder syndrome.
During our examination we found numerous, common accompanying symptoms.
Other complaints
Personality/Traits
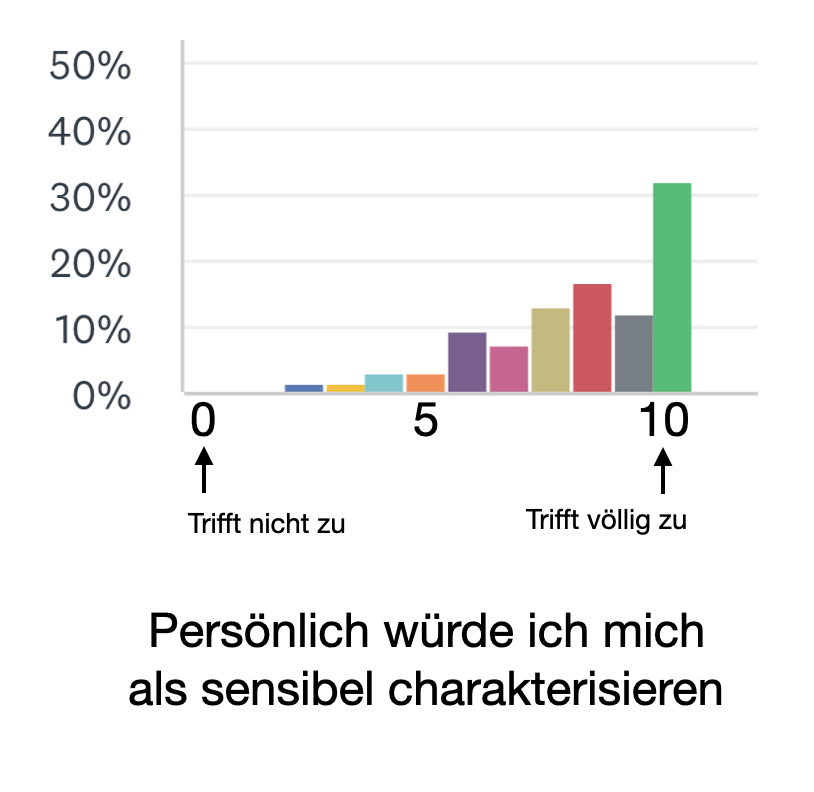
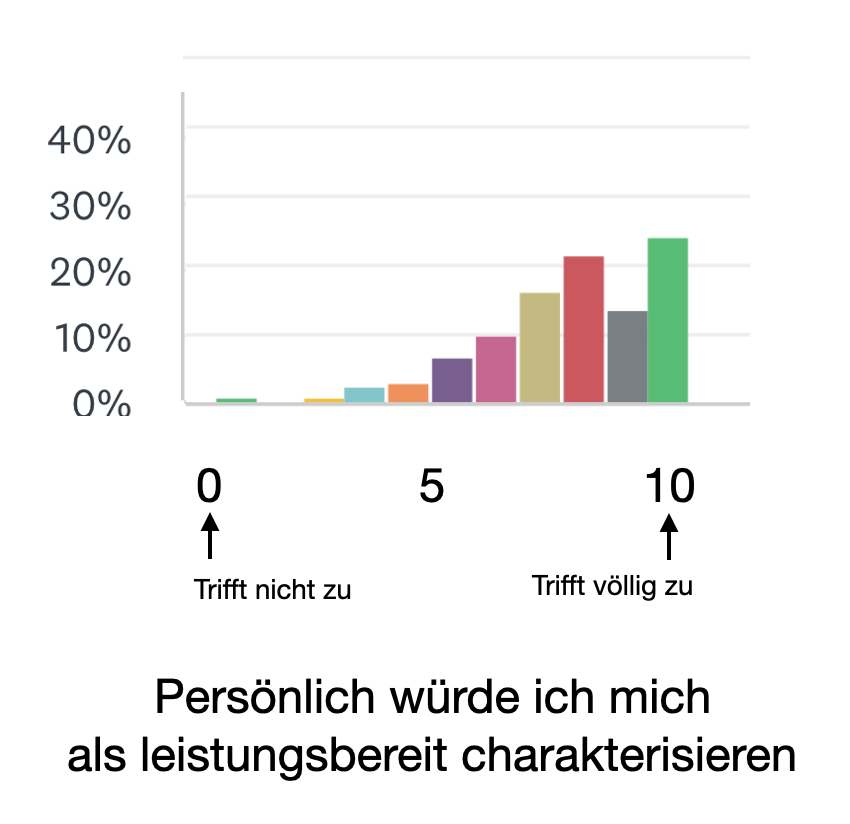
In the therapy of vulvodynia patients, we always notice that a certain form of personality dominates. They are often sensitive achievers who are perhaps not necessarily "go-getters" but rather reserved and more cautious.
During the survey, we were able to confirm this. The vast majority describe themselves as sensitive, willing to perform and precise!
Sensitivity
Readiness to perform
Accuracy
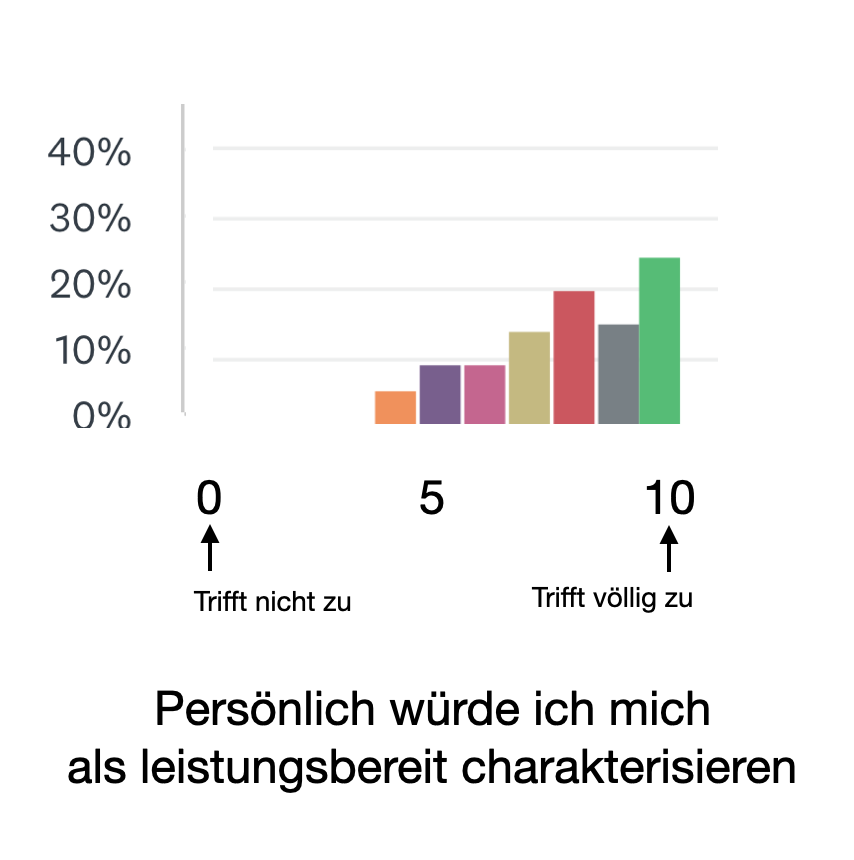
357 participants each
Diagnosis
During diagnosis, organic (e.g. gynecological, neurological) diseases should be excluded. Of course, this includes a gynecological examination.
There is a general hypersensitivity (med. hyperalgesia) or a stimulus that is not painful in itself (e.g. touch, cold/heat) is experienced as painful (med. allodynia).
If the pain occurs without external cause (e.g., touch with a cotton swab), then the diagnosis is generalized vulvodynia.
If the pain occurs only when touched (e.g., with a cotton swab), then the diagnosis is "provoked vulvodynia". If this was already the case since menarche (1st period), then a "primary" disorder is present, otherwise one would speak of a "secondary" disorder.
Criteria
- Pain and burning in the vulva area. Intensification with pressure or touch (traffic, cycling, clothing).
- No or only slight redness
- Exclusion of other diseases (e.g., vulvovaginal candidiasis, genital herpes), neurologic (e.g., herpes neuralgia, spinal nerve compression), dermatologic (e.g., lichen planus, lichen sclerosus), or neoplastic diseases (e.g., vulvar intraepithelial neoplasia)
- Duration over three/six months
Exclusion of various diseases
In clarifying the causes, a number of diseases should be investigated or excluded. Among them are the following:
- Organic diseases of the vulva (includinglichen sclerosus).
- Diseases of the nerves (neuropathy) in the area of the small pelvis
- Transmitted pain (radiation) from other areas of the lesser pelvis
- Malfunctions of the muscles of the lesser pelvis
- Depression is said to be more common in sufferers, although it is unclear whether this is a cause or a consequence of the symptoms (see this issue withfibromyalgia)
- Skin diseases
- Fungal diseases
Therapy in general
Body care should be very careful.
- It is recommended not to use deodorants or the like.
- Be careful with perfume, soaps, shampoo or similar.
- The vaginal entrance should be cleaned with water carefully if possible, gently patted dry and then cared for with a mild skin oil or vegetable oil.
- If tampons are irritating, cotton pads are more beneficial.
- Lubricants are recommended during intercourse. After intercourse, cold packs (don't overdo it) can be helpful to reduce swelling.
- After urination, it may be useful to clean the vulva with water.
Caution with ointments, etc.
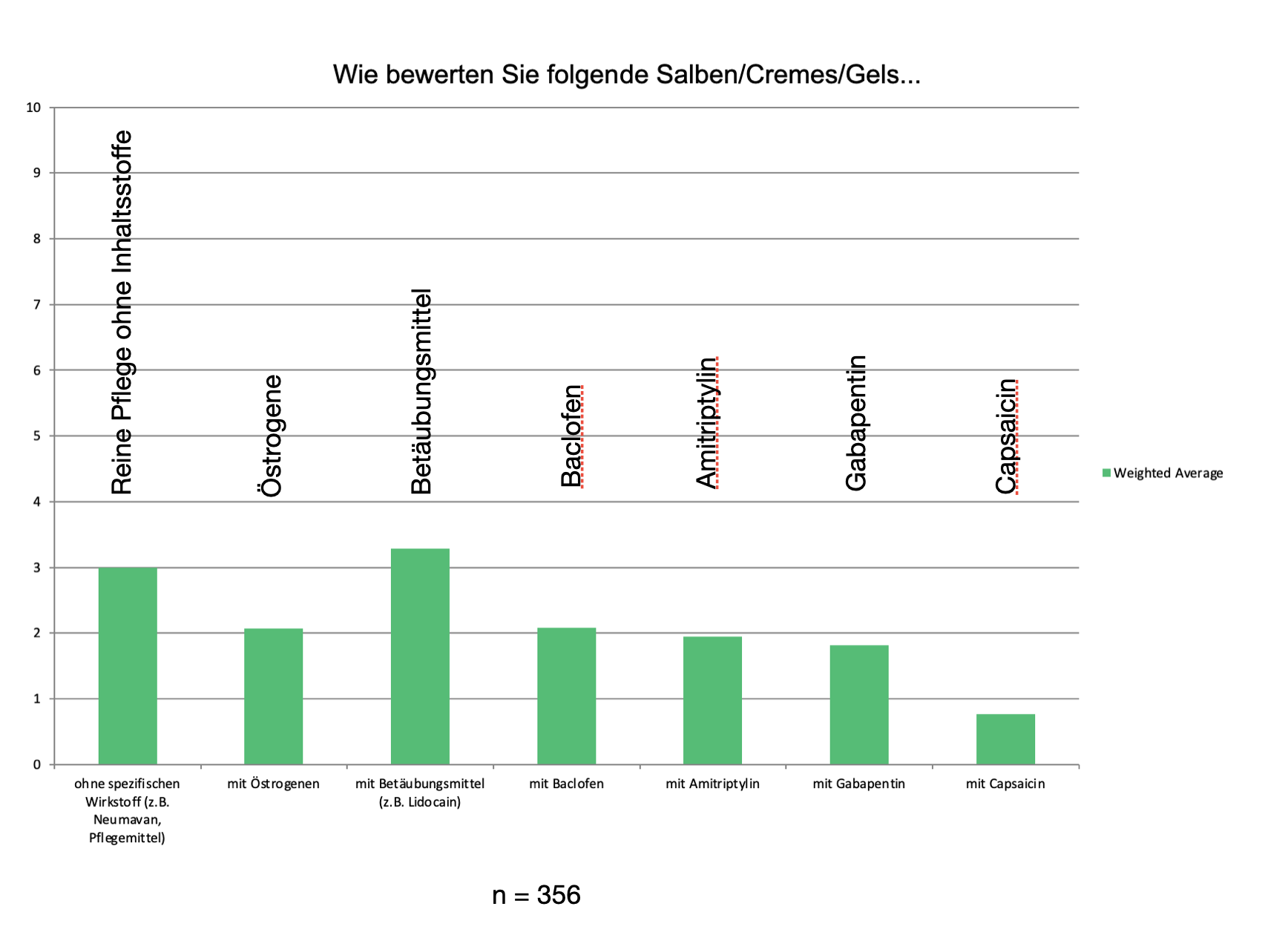
Very many ointments, tinctures are recommended.Very often, however, the local medications lead to further sensitization and thus worsening of the symptoms. In short, the burning sensation is intensified. Therefore, often the first therapeutic step is to discontinue all ointments, etc..
However, there are situations where certain preparations can be helpful. However, you should discuss this with your doctor. The following may be worth trying:
- Local anesthetics. These can be applied, for example, 30 min before intercourse. Overnight application on a cotton ball is also helpful, but only occasionally.
- Combinations of local anesthetics (e.g. ointment from the pharmacy)
- Pure Vaseline or similar care products have been used with success in individual cases.
- Ointments to promote blood circulation are effective in individual cases
- Combination of antidepressants and painkillers reduces pain in individual cases.
Overall, the participants in our survey were very skeptical about the vast majority of local remedies. The "best" results were achieved by pure care products, but here, too, experience is extremely modest.
Only a three on the 10-point scale was achieved by the "best" ointments.
We therefore do not recommend ointments. Pure care products with as few ingredients as possible or oils such as coconut oil are most likely to be used.
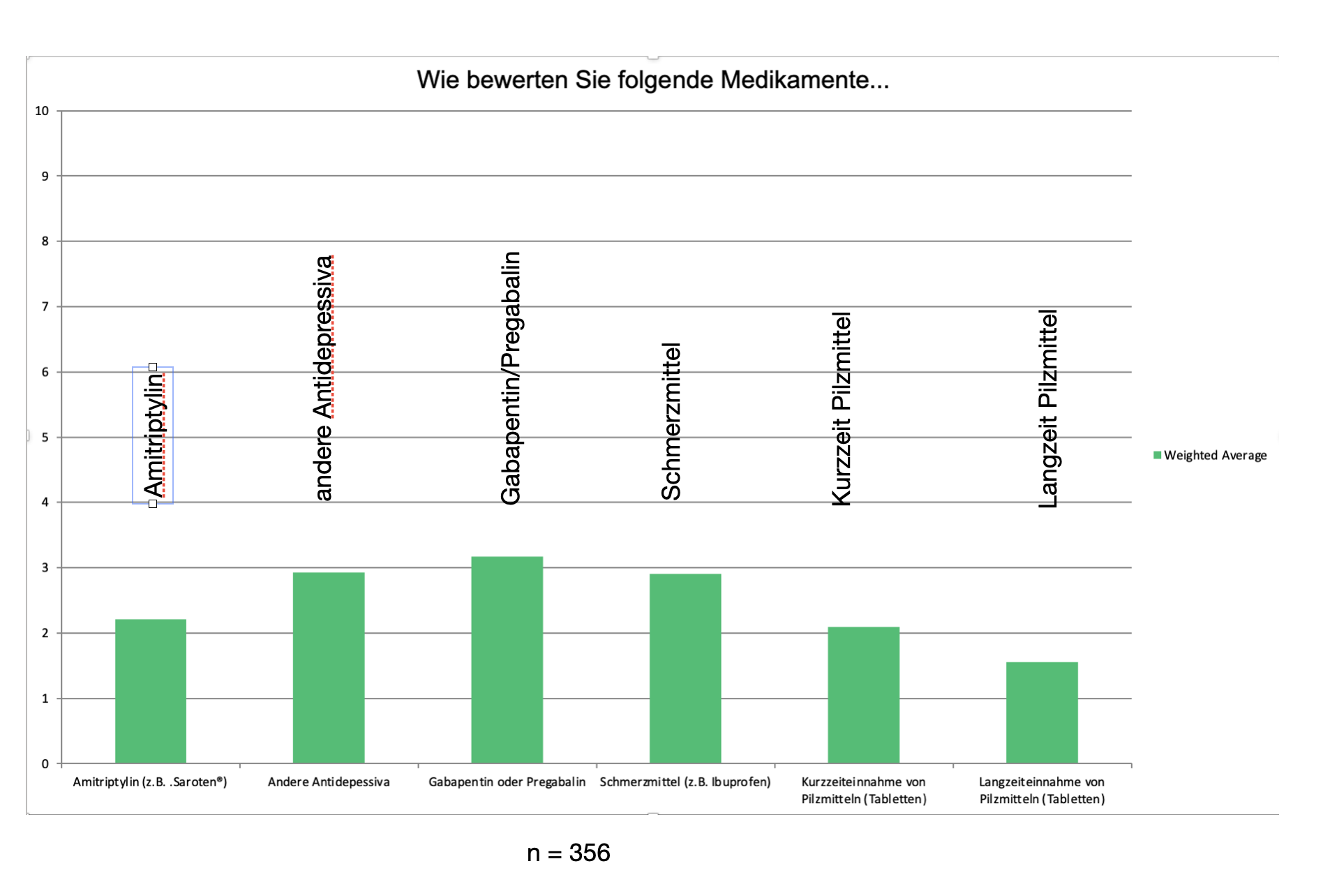
In general, the effectiveness of drugs is very limited, as our survey showed. Nevertheless, some preparations should be mentioned here.
Antidepressants: These drugs are effective (in high doses) against depression. In very low also against pain. In practically all central sensitivity disorders (irritable bowel, fibromyalgia, irritable bladder, etc.) these preparations are used with success. We then give our patients specific recommendations for a specific substance.
Since most patients are very sensitive even to medications, it should be started low and then increased as needed ("start low, go slow"). We prescribe antidepressants as drops and start with a single drop in some water in the evening. In the following evenings, the dosage can be increased slightly drop by drop. The sleep becomes calmer and deeper at the same time. In the morning, sufferers should feel well-rested but not dizzy. (Amitriptyline is available only on prescription, as always: consult your doctor).
Important: The effectiveness of antidepressants is not based on the antidepressant effect but on the pain-relieving effect.
Anticonvulsants:Anti-epileptic drugs also have an effect on vulvodynia. They dampen the increased irritability of the nerves. They must be individually dosed and taken over a period of time to have an effect.
Nerve blocks:Experience with blocking nerves by injections is very variable. Sustained success is rare.
Cortisone:Cortisone has not been shown to be helpful - even as an infection into the pain region.
If you look at the evaluation below, you will unfortunately see that drugs are generally viewed extremely critically in our survey. The blue bar indicates in each case when the preparations are rated as not very helpful (0-2). The green bar refers to the assessment helpful (8-10).
Surgical interventions
Various surgical procedures are performed in which painful districts are partially or completely removed. From our point of view, we would strongly advise against this. There must be very good arguments for surgery before it should be considered for "normal" vulvodynia. We have seen patients in whom the symptoms continued unchanged even after complete removal of the labia.
The same is true of very painful therapeutic procedures, which in our experience lead to an increase in sensitivity and thus more pain. Likewise, all procedures that are associated with strong anxiety are unfavorable.
Psychotherapy
Psychotherapy alone (without accompanying other measures) is usually not sufficient to achieve lasting pain reduction. In combination with other methods (e.g. multimodal therapy), psychotherapy can be a very valuable element, e.g. to reduce anxiety and talk about partnership problems.
Evaluation of individual therapy proceduresb
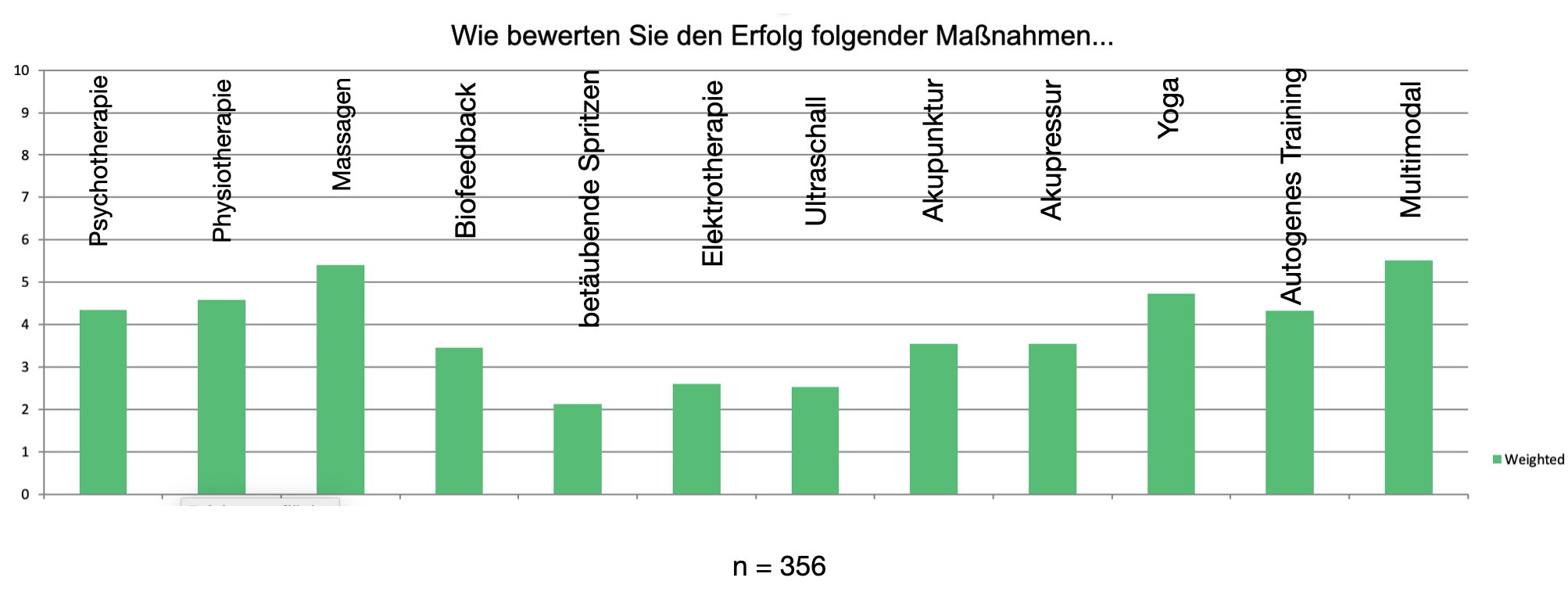
In our survey, multimodal therapy scored best. In our case, this also includes massages - which were also rated very highly. Similarly, body-related procedures were rated significantly better than medications or intrusive procedures such as local anesthesia through injections.
Multimodal therapies were rated best.
Multimodale treatments
More than one therapy method
With such complex complaints as vulvodynia syndrome, single measures are often not very successful. This is not peculiar to this pain disorder. In the case of other functional complaints, too, a comprehensive therapy concept is usually applied, consisting of several building blocks. In addition to medication, this usually includes: Psychotherapy, physiotherapy, exercise and self-help.
In vulvodynia, too, it is necessary to use such multimodal therapies, at least in cases of prolonged course or severe complaints. Prof. Mendling (FRAUENARZT 5 (2014) No. 5 and 55 (2014) No. 6) puts it this way: "Multimodal pain therapy, which is described for fibromyalgia but should also be used for vulvodynia/vestibulodynia, requires interdisciplinary cooperation between the gynecologist and at least one psychiatrist, psychologist, or psychosomatician and must include at least three of the following therapeutic methods simultaneously: Psychotherapy, specialized physical therapy, relaxation techniques, occupational therapy, medical exercise therapy, sensorimotor training, workplace training, art and music therapy or other exercise-based therapies, and biofeedback therapy."
What helps beyond creams and pills?
From our point of view, it is a matter of reversing the sensitization process. In this process - as research results from other fields also show - a hypersensitivity of the stimulus processing of the complete nervous system plays a role:
- Increased sensitivity receptors of the mucosa.
- Slight inflammatory activity of the mucosa
- Increased transmission in the spinal cord
- Increased conduction in the brainstem
- Increased attention in the somatosensory cortex (where stimuli are perceived)
In addition, there is anxiety and tension, sleep disturbances and other functional complaints. Irritable bowel and bladder complaints or swelling (edema) in the area of the pelvic floor have a particularly unfavorable effect, as the regional nerves of the pelvis are additionally irritated in this way.
False alarm
Essential to therapy is the fact that it is not possible to consciously decide to ignore pain. True, it is typical that in phases of distraction or during acute stress the complaints subside. But afterwards they return (usually more strongly).
If the symptomatology has existed for a long time, then the body does not expect anything good from this region and pays scrupulous attention to every signal coming from the area of the pelvic floor. It is transported to the consciousness with priority. In principle, this is not meant badly, since the body - erroneously - assumes: danger is imminent here!
Fatal sparing
Most affected women find out in the course of time that above all one way protects them from the persistent complaints: Protection and avoidance of stimuli. If there are no - or as few as possible - stimuli, then only little can reach the brain.
But as understandable and sensible as this approach may seem at first glance. It has a fatal consequence: the stimulus threshold goes further down, sensitivity increases. The more stimuli are avoided, the more sensitive the region becomes. This process is sometimes referred to as "pain memory."
But what can a way out look like when every little stimulus triggers discomfort and avoiding stimuli actually makes symptoms worse in the long run?
It has taken us a long time to find a sensible answer. It is: The nervous system must learn that signals are not threatening and that the increased attention is therefore not necessary.
When stimuli from the vulva area are repeatedly coupled with the feeling of relaxation and safety, the nervous system slowly moves out of the permanent state of alarm. The more frequently signals are judged to be non-threatening or even pleasant, the sooner they are faded out again. The stimulus threshold rises.
Graduated desensitization
These basic considerations apply to many regional pain syndromes. And even in generalized pain (such as fibromyalgia), these processes are crucial.
In vulvodynia, direct touch by the therapist is forbidden for obvious reasons. Often the area is so sensitive that even the smallest stimuli cause burning/pain.
We therefore try to reach the target in a "roundabout way". In most cases, the increased sensitivity is not only present in the vulva area. It can usually be found in other parts of the body, in the gastrointestinal tract, in the heat/cold perception or in other forms.
Therefore, we first begin to treat the body. Gentle massages of the back or neck, heat, relaxation procedures, breathing therapy, sleep hygiene, dietary changes and other procedures that almost fall into the category of "wellness" are used to lower the general tension and hypersensitivity to stimuli.
In a second step, hardening procedures are also used. The body is to learn that even more powerful stimuli are by no means threatening.
Finally, indirect stimuli are applied in the area of the pelvic floor: vibration stimuli on the vibration plate, pelvic floor exercises and similar procedures tell the nerves there: "There are stimuli here, but they are not dangerous!"
It's not necessarily the length of therapy that matters but the number of repetitions. The nervous system needs to experience again and again, "These stimuli are not threatening!"
The more comprehensive this experience is, the more effective the therapy. If as the pressure and touch sensors, the heat and cold sensors, the muscle nerves, the nerves of the gastrointestinal tract and the bladder all have the same positive experience, then a new state is established in the body: The stimulus threshold goes up.
We usually treat briefly but very intensively. This means that we perform an abundance of applications over two weeks. In the beginning this can be exhausting even if the single applications are very pleasant. The background: daily therapies over two weeks have proven to be much more effective than one therapy session per week over 3 months.
In addition, measures to improve sleep, the gastrointestinal tract, relaxation and breathing or applications according to individual cases.
In very many cases, the pain subsides within a short period of time. How far we get in two weeks depends, of course, on the individual case: How pronounced are the complaints? What other symptoms are present? How strong is the inner uncertainty?
During this time, we also teach our patients how to proceed with self-help. The goal is to achieve the greatest possible autonomy, i.e. to be able to cope with the symptoms themselves without professional help.
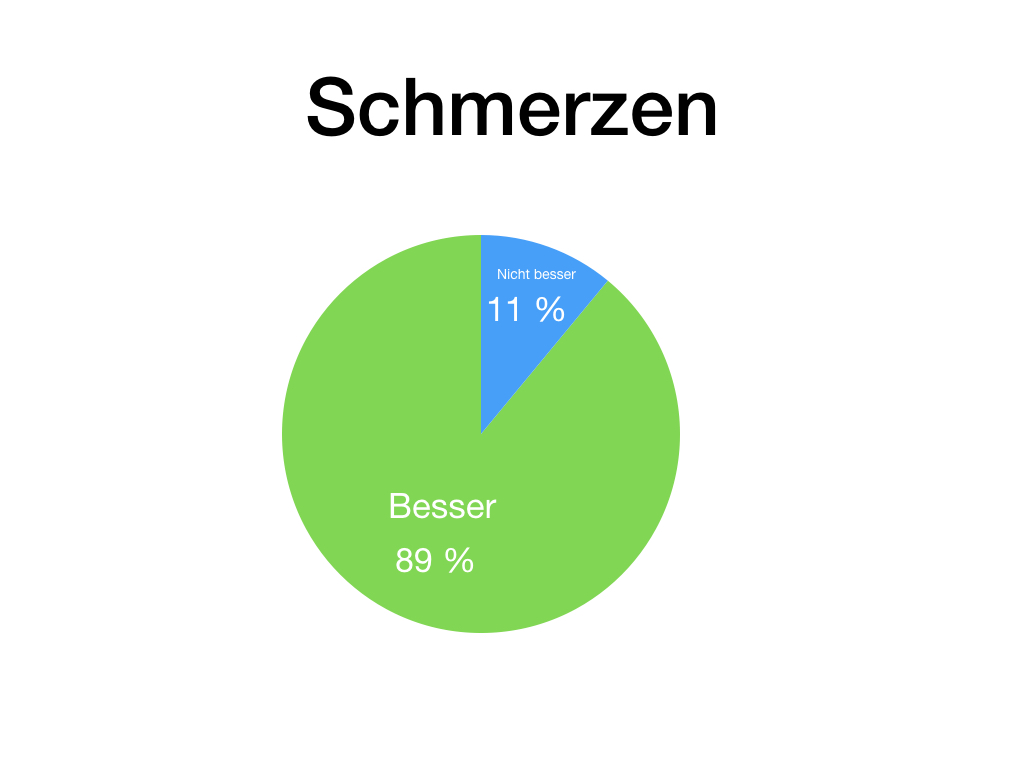
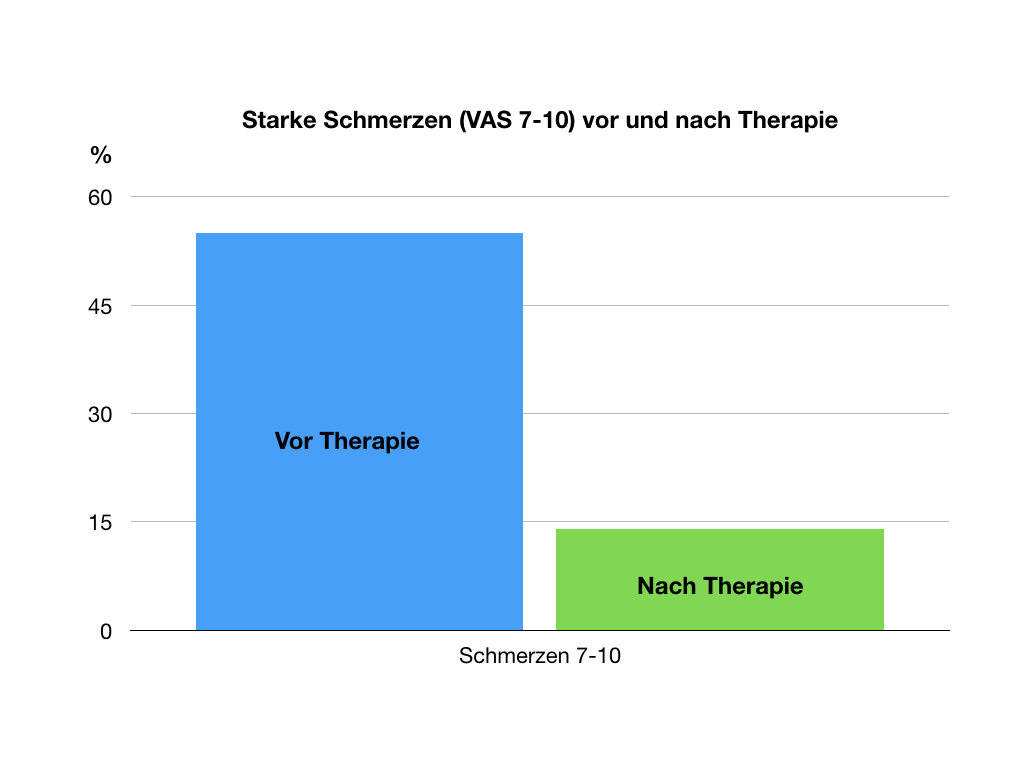
As a rule, freedom from pain cannot be achieved with 12 days of therapy. Nevertheless, we are seeing very pleasing developments, particularly with regard to severe pain. This has been reduced considerably from 55% to 14% of those affected! (pain intensity VAS 7-10). The progress was even more significant for the strongest pain level "10". This decreased from 26% to 3%.
Self-help
Vulvodynia syndrome is not only a burden because of the pain, but also because of the helplessness associated with it. If neither painkillers nor therapy methods by specialists bring about relief of the symptoms, then many of those affected find the feeling of being at the mercy of others particularly agonizing.
For this reason, it is important for us to provide self-help methods that can bring about tangible relief. As soon as affected women have the impression that they can really achieve something themselves, the fear and tension diminish and this is usually associated with a decrease in pain/burning.
We have tried a number of procedures in recent years. For a while we used biofeedback with local electrical stimulation. However, we tended to move away from this, as the electrical stimulus came across as unpleasant and threatening to many women, thus increasing sensitization.
In contrast, we found the targeted instruction of pelvic floor training, which can be practiced at home, to be effective. Our physiotherapists explain the individual exercises in detail.
Very helpful is the use of vaginal dilators, which we prescribe to our patients at the expense of the statutory health insurance (we have such sets in stock). This training can then be performed daily (exclusively at home). Many women are surprised how unproblematic this training is.
Another self-help method is breathing therapy. Here we guide with exercises and with a carbon dioxide controlled biofeedback. These exercises are described by many patients as central to the progress of therapy and can be continued at home.
Other elements may include range-of-motion exercises, such as trampolining, to gradually return weight to the pelvic floor.
In general, at the end of each therapy session, our patients have a whole set of procedures with which they can then continue to practice at home.
Videos affected
Please see the important notes that apply to all affected person videos.

