Pain, swelling, unstoppable weight gain, bruises and a persistent suffering of the figure.
And nothing seems to help: Exercise and diets fizzle out ineffectively, and even doctor-prescribed measures like compression stockings or lymphatic drainage do little to change the discomfort.
What is it? Why does it not get better? Is there no real help?
What is lipedema?
What actually is "lipedema"?
Lipedema", literally "fat swelling", is understood to be a symmetrical increase in subcutaneous fatty tissue. It mainly affects both legs, the hips and - somewhat less frequently - the arms. The affected body regions are painful to the touch and there is a tendency to bleeding ("bruising", med. "hematoma").
The clinical picture occurs almost exclusively in women. In men, it can develop, for example, if they are very overweight or after therapy with female hormones.
Definition according to ICD 10
"Lipedema is a mostly progressive (=progressing) disease characterized by a symmetrical subcutaneous fat tissue proliferation predominantly of the lower, rarely of the upper extremities. In addition, there is edema formation, often with tension, pressure and touch pain, as well as a hematoma tendency (=blue spots) after minor traumas (=injuries). In advanced stages, lymphostatic edema may develop."
Why sports and diets do not help!
Basics: About the lymphatic system
The sewage treatment plant of the body
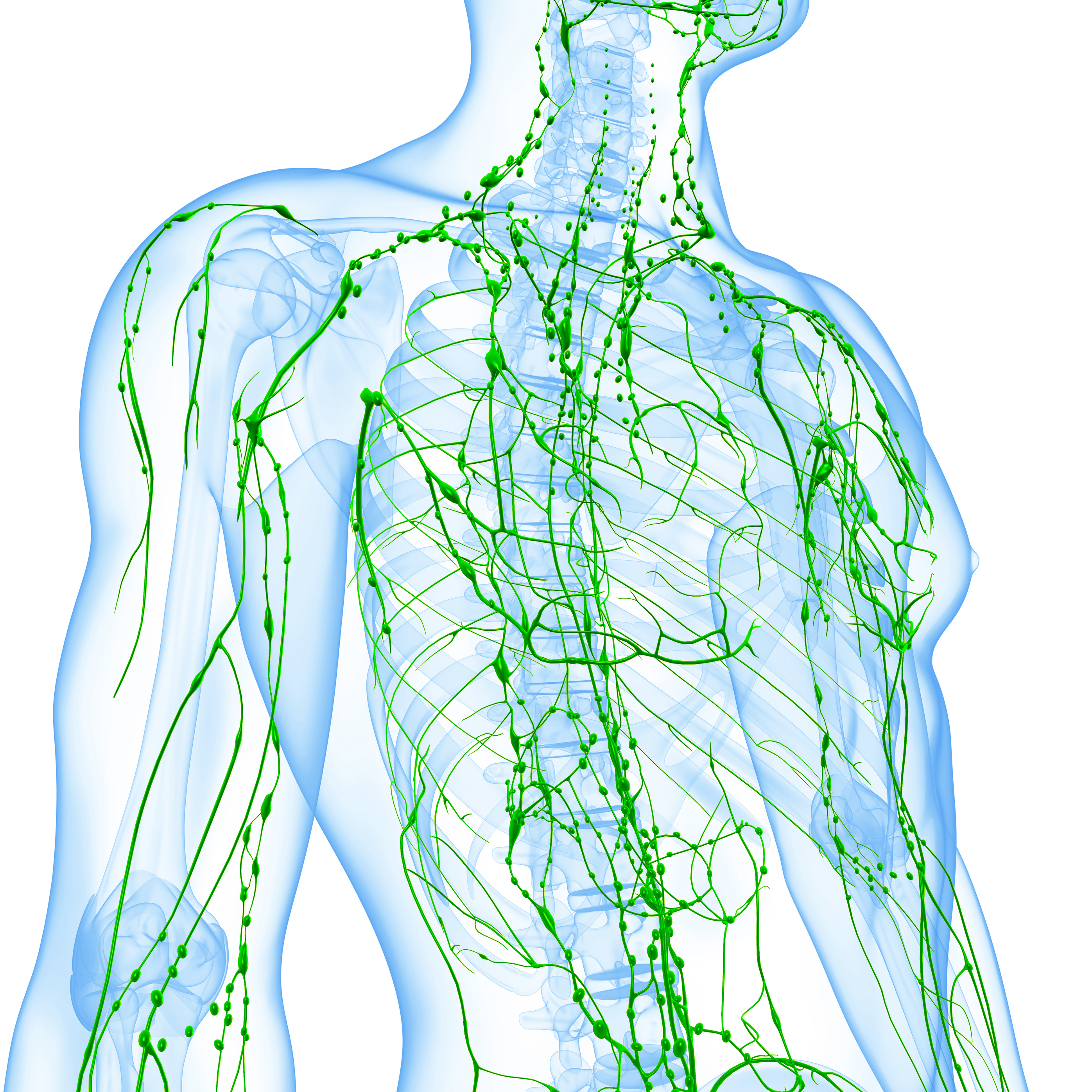
Everyone knows what the blood circulation is good for. But what is the lymphatic system for? You can feel the lymph nodes in your neck when you have a cold or angina. But the lymphatic system as a whole, what belongs to it in detail and what function it has, even medically experienced people often have to pass.
Drainage and drainage
Not all living creatures have a lymphatic system. Fish get along brilliantly without one. However, we humans, just like all mammals and birds, need it.
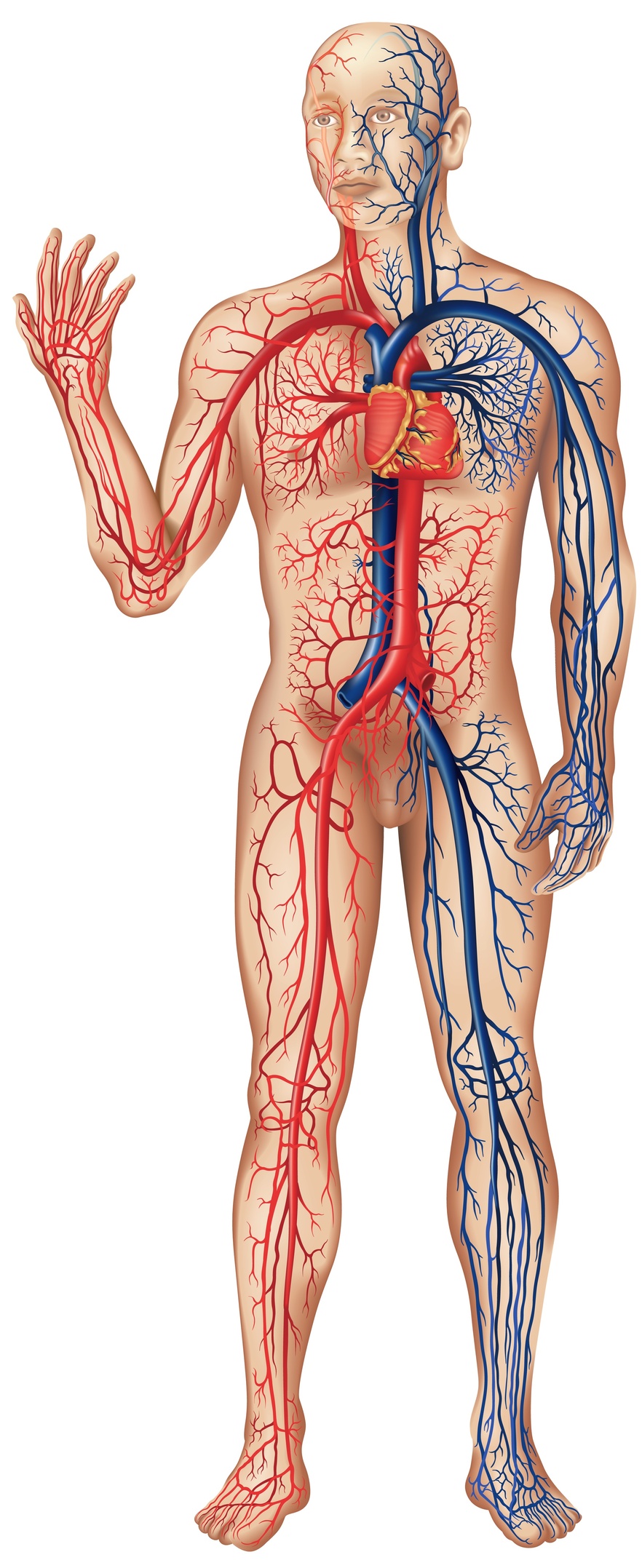
The lymphatic system is therefore a one-way street that starts in the periphery in almost all tissues of the body. It collects all the "special waste" there and empties it into the superior vena cava just before the heart. Thus the cycle is closed. Thus, all higher organisms have a system, namely arteries, that leads away from the heart and a double vascular system, namely veins and lymphatic vessels, that transport blood and lymph back to the heart.
This drainage or draining function of the lymph is one of its main jobs. Whenever fluid becomes trapped between cells, for example in the case of injury or inflammation, it springs into action to ensure that it is absorbed and safely removed. The effect of the failure of the lymphatic system became visible in an animal experiment. If the lymphatic system of only one leg is completely cut off, death will inevitably occur within 24 hours!
Our problem: upright gait but no fur!
Compared to other living beings, the lymphatic system is of special importance for humans. The first reason is its upright gait, which distinguishes humans from their relatives, the apes. As favorable as this uprightness was for development, it came at the price of increased pressure on the blood vessels in the legs. In humans, these are under constant pressure and allow more fluid to seep into the tissues of the lower legs and feet. If we would move on all fours like our animal ancestors, you could read over this text.
The second reason also has to do with our evolutionary history. Humans lost most of their hair and moved through savannahs and forests as "naked apes". However, a coat is not only dressing, it mainly protects against cold. In order not to freeze to death, humans developed a thick layer of fat in the subcutis that protected us from hypothermia instead of fur. This subcutaneous fat could not be too thin. To replace a fur of one centimeter height, one needs a fat pad four centimeters thick! No other living creature, not even the fat pigs, have such a pronounced fat coat, even in the area of arms and legs. This provides us humans with excellent protection against cold nights outdoors. But the protection against the cold also has its disadvantages, and now the subject of "lymph" comes into play.
The thick subcutis consists of very loose fatty tissue. Unfortunately, fluid is also easily deposited there. The danger is that so much fluid accumulates that swelling, an edema, occurs. To prevent this, the human body needs an efficient additional drainage system, the lymphatic system.
Three factors favor the development of edema in humans:
- High blood pressure
- Upright gait
- Thick subcutaneous fat
The lymphatic system serves to transport away all substances that develop between the cells in the connective tissue. In addition to fluid, these are mainly proteins, cells, but also foreign and harmful substances. In addition, it has a crucial importance for the function of the defense.
The big difference between blood vessels and the lymphatic system is that the lymphatic system forms only a semicircle. It starts blindly in the periphery and transports the lymph back to the heart.
(copy 6)
The way of the lymph
Fluid, salts and especially protein leave the bloodstream and accumulate between the cells. One reason for the leaking capillaries is the overpressure that exists in the blood vessels. Another reason is as follows: along with the proteins, many vitamins and nutrients also leave the bloodstream to nourish the cells.
But then where do the fluids and nutrients go? For osmotic reasons, their way back into the blood is blocked. Once they leave, they can never go back there. In a short time, they would accumulate there and lead to disaster. This is where the lymphatic system steps in: it has the function of a drainage system that absorbs the leaked substances such as protein, cells, salts and fluid and returns them to the bloodstream. It is a one-way street that starts in the periphery in almost all tissues of the body. It collects all the "special waste" there and empties into the superior vena cava just before the heart. Thus the cycle is closed. Thus, all higher organisms have one vessel (the arteries) that leads away from the heart and two vessels, veins and lymphatic vessels, that carry blood and lymph back to the heart.
This drainage function of lymph is one of its main functions. Whenever fluid accumulates between the cells, for example in the case of injury or inflammation, it comes into increased action and ensures that it is absorbed and safely removed.
Anatomy
The lymphatic system thus transports the lymph out of the space between the cells, the connective tissue. There, the smallest lymph capillaries take up the fluid and lead it to the larger collecting vessels (so-called "collectors"). These, in turn, flow into lymphatic trunks, which then finally end just before the heart in the superior vena cava.
Interspersed in the lymphatic channels are the lymph nodes, which can often be felt in the bends of the arms and legs. Each person has about 500-600 of these lymph nodes. Lymph is concentrated in them, and most of the fluid is already released into the blood at this point. The lymph nodes work very effectively in this process. Every day they produce a concentrate of about 2 liters from 1000 liters of primary lymph, which is finally emptied into the superior vena cava via the large lymphatic trunks.
Lymphatic capillaries
The lymphatic system originates in the connective tissue. It serves to drain and dispose of all superfluous substances, which taken together are referred to as the "lymphatic load". In addition to protein, these are mainly water, fat, numerous cells, bacteria and pollutants of all kinds.
All of these substances collect in tiny tissue crevices located upstream of the lymphatic system proper. They are called the prelymphatic (pre=before) channel system. They can perhaps be compared to the furrows left in the soil by rain as water drains through them.
The first true lymphatic vessels are the lymphatic capillaries. They can most readily be thought of as drainage pipes in a marshy meadow. Like such pipes, they have innumerable openings into which water, protein and cells can flow virtually unimpeded. The pores are closed only by small oscillating flaps or cusps.
The lymphatic capillaries do not simply lie in the "sump" of the connective tissue, they are suspended in it by a network of filaments (so-called filaments). The more fluid there is in the connective tissue, the more these filaments pull on the cusps. These open and fluid flows into the lymphatic capillaries. This process continues until the pressure inside the lymphatic vessel is high enough to close the valve again. Now, another previously closed valve opens at the exit of the lymphatic capillary and pumps the lymphatic fluid into the lymphatic duct that continues on. Thus, the more fluid that accumulates, the faster it is disposed of.
Stage I lymphedema

In stage I lymphedema of the foot, the permanent dents are typical, which appear on thumb pressure and disappear after some time or elevation.
In later stages, the dent does not regress.
Lymphatic collectors
Once the fluid has been successfully absorbed by the lymphatic capillaries, the next step is to collect it. Collecting vessels or "collectors" serve this purpose.
They not only collect the lymph, but also ensure that it is transported further with the necessary pressure. To do this, the collectors have a layer of muscle and a system of valves, similar to venous valves.
Every 10 seconds, the muscles of one of the centimeter-long segments contract. This would allow the lymph to flow both forward and backward. But the backward flow is inhibited by two leaflet valves that close rapidly. In this way, there is an effective and continuous flow of lymph from the periphery to the center. The lymph flow passes through about 100 of these pairs of valves until it finally reaches the heart.
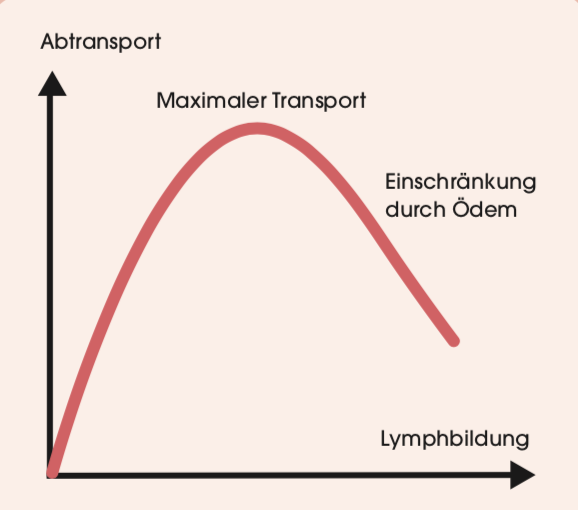
This system of valves and vascular muscles is thus the actual "heart" of the lymphatic system. It pumps the lymph forward, just as the heart circulates our blood. Many of the laws that apply to heart action therefore also apply to lymph transport. Thus, the more filling pressure there is, the more effectively lymph transport works. The more lymph there is, the better it is transported.
This transport is also supported by muscle activity. When we go for a walk or do sports, the muscles rhythmically squeeze the lymph vessels. This is another way in which the valves become active and help the lymph flow.
Pulsation of the arteries (arteries) has a similar effect. Since they are often packed together with the lymph vessels in a vascular-nerve bundle, their movement is transmitted to the lymphatic system. The more we exert ourselves, the stronger the pulsations and thus the lymph flow.
The interplay of breathing, which at one time builds up negative pressure and then positive pressure, also supports lymph flow. Even the movement of the intestines (intestinal peristalsis) improves it, since the movement of the intestinal muscles activates the huge intestinal lymphatic system. In short, any movement promotes lymph flow!
Lymphatic trunks
All lymphatic collectors finally flow into the largest lymphatic vessel in humans, the thoracic duct (med. Duktus thoracicus). The term "milk duct" was chosen because the approximately 40 cm long collecting vessel is filled with fat droplets after a meal. These then cause the otherwise clear lymph to appear whitish-cloudy.
The mammary duct also contains a system of valves that facilitates transport. It ends at the superior vena cava just before the heart. Similar to a water jet pump, the excretory duct projects into the vein at an angle, which facilitates the emptying of lymph.
Generally, the thoracic duct collects all the lymph from the legs and left arm and transports it to the left superior vena cava. The lymph of the right arm usually empties separately into the right superior vena cava. However, here the differences from person to person are considerable.
Lymph nodes
If the lymph vessels transport the "waste" or even "hazardous waste," then the lymph nodes are the body's sewage treatment plants. Every person has 600 of these little marvels. Particularly many are located on the neck, armpits and groin, as well as along the gastrointestinal tract (about 200 there).
Most lymph nodes are small, that is, smaller than one millimeter. However, they can enlarge when they are particularly stressed, growing up to three centimeters. This is usually the result of an infection. Everyone knows this with the swollen throat lymph nodes during a pharyngitis.
All lymph nodes have numerous feeding but only one draining vessel. This already reflects one of their main tasks, the concentration of lymph fluid. In this process, the small purification plants do an incredible job: they manage to produce a concentrate of about 2 liters from 1000 liters of primary lymph (this is the fluid that has been absorbed by the lymph capillaries). Only this residual amount returns to the blood through the mammary duct at the end. However, this amount may increase if more lymph is produced in the body. 20 liters even 50 liters can be produced in the course of a day during severe diseases.
However, lymph is not only concentrated by the lymph nodes, but also cleansed. Foreign bodies, bacteria, cellular debris and other components of the lymph are broken down or deposited to protect the highly sensitive blood from damage. In smokers, for example, the lymph nodes of the lungs turn deep black because of cigarette pollutants.
Of course, the function of the lymph nodes is particularly important for the immune system. Bacteria are neutralized in the lymph nodes by specialized cells, and antibodies against viruses are produced at the same time.
Lipedema and adipose tissue
Energy storage
80% of body fat is stored directly beneath the skin. As already illustrated, we as humans need this insulating depot because we do not have a warming coat like our ancestors, the apes. Fat insulates against cold, protects against impact, and is what first gives the body a smooth, aesthetic appearance.
Between 15-25% of the body weight in a normal weight woman should be fat tissue (in men 10-20%). It can also be a few percent more, without having to speak immediately of overweight. This energy store is sufficient to last for a good month without any food, if sufficient fluids are consumed. If you had to store this amount in the form of carbohydrates, your body weight would double - not a pleasant idea.
Building material
In addition to the so-called depot fat, e.g. the subcutaneous fat, there is also a building fat. It is found on the palms of the hands, the knee joint, the cheeks or even behind the eyes. The task of this building fat, as the name suggests, is mechanical stabilization. It is not attacked at first during weight loss. It is only broken down during massive hunger states. A person with hollow cheeks and deep-set eyes is thus the symbol of emaciation.
Warming adipose tissue
Little known is another type of fat, brown fat. It is most common in the animal kingdom, for example in rodents or animals that hibernate. Unlike white fat, brown fat has thousands of tiny energy factories (mitochondria) in each cell that are capable of generating a great deal of heat. With the help of brown adipose tissue, a Siberian hamster, for example, manages to successfully defy the proverbial Siberian cold. The fatty tissue keeps it comfortably warm while it dreams of spring in deep sleep.
Adults have only tiny remnants of this type of fat in the armpits and along the large vessels. Infants are better endowed in this regard, and it makes sense, since they are less able to actively warm themselves through movement. The brown fatty tissue they have, especially in the back, warms them like an electric blanket.
Classification stages
Classification: Stage I
In the early stages, there is usually no or no significant excess weight. Patients complain of tightness in the legs. After prolonged standing or sitting, e.g. car journeys, the complaints increase. In the evening, the stockings stand out on the lower legs. The legs are more sensitive to pain, and hematomas, bruises, often occur even with slight bumps.
Thighs, hips and lower legs increase somewhat in volume. The arms are less frequently affected. The skin looks smooth on the outside, but deep down one can already feel an uneven distribution of fat in the form of small nodules.
Unlike watery edema, pressure with the thumb does not leave a permanent dent. On the contrary, the tissue is plump and elastic.
On palpation, the irregular distribution of fat and the small nodules are noticeable.
Stage I
Stage II
Especially after a phase of weight gain, there is a further thickening of the skin. This now shows visible irregularities and retractions, which are often called orange peel skin, "cellulitis" or "cellulite".
The last terms are not used in medicine, as the suffix "-itis" is reserved for inflammations. However, lipedema is not in itself an inflammation, even though an inflammatory component in the connective tissue plays a role. This is at least partly responsible for the increased fluid leakage.
Stage III
In the final stage, the skin is further thickened and hardened. The skin is now not only wavy, but shows pronounced wrinkles and lobes that make walking difficult when they are very pronounced on the inner thighs and knees. Now it is particularly noticeable that hands and feet are not affected and the swelling starts abruptly at wrists and ankles.
The skin now feels coarse and hardened in depth, and in some places noticeably cool. Especially on the outside of the thighs ("riding pants") and on the hips, the skin can be very thickened.
"Stage IV"
In lipedema, hands and feet are completely spared from swelling. They remain slim. However, in advanced forms of lipedema, there is also increased water retention in the back of the feet and toes or back of the hands and fingers.
The skin folds on the toes become so thickened that they can no longer be lifted off. This phenomenon is called "Stemmer's sign" (suggested by Renate Stemmer) and is characteristic of lymphedema. Now it is present as a combination of lymphedema and lipedema.
Especially if the lipedema exists for decades, then slowly the feet swell as well. The skin folds of the backs of the feet and toes become impossible to lift off. Now lipo-lymphedema has developed, which is sometimes called "stage IV" lipedema.
Stemmer's sign
"Elephantiasis"
Especially in significantly overweight female patients, the disease can lead to extremely severe changes. This stage of the disease is then called "elephantiasis" (elephant legs). The fat folds are so extensive that walking becomes practically impossible and the affected persons require constant assistance.
Other classifications
In medicine, there are often different classifications in parallel. Here are two further attempts to create clarity and order. However, there is probably no deeper biological cause behind them. They are merely descriptions of the appearance.
Type classification 1
- Type 1: Hips
- Type 2: Hips and thighs
- Type 3: hips, upper and lower legs
- Type 4: Arms
- Type 5: Lower legs
Type classification 2
- Upper leg type
- Lower leg type
- Calf type
- Whole leg type
- Upper arm type
- Forearm type
- Whole arm type
Lower, upper, gank body type
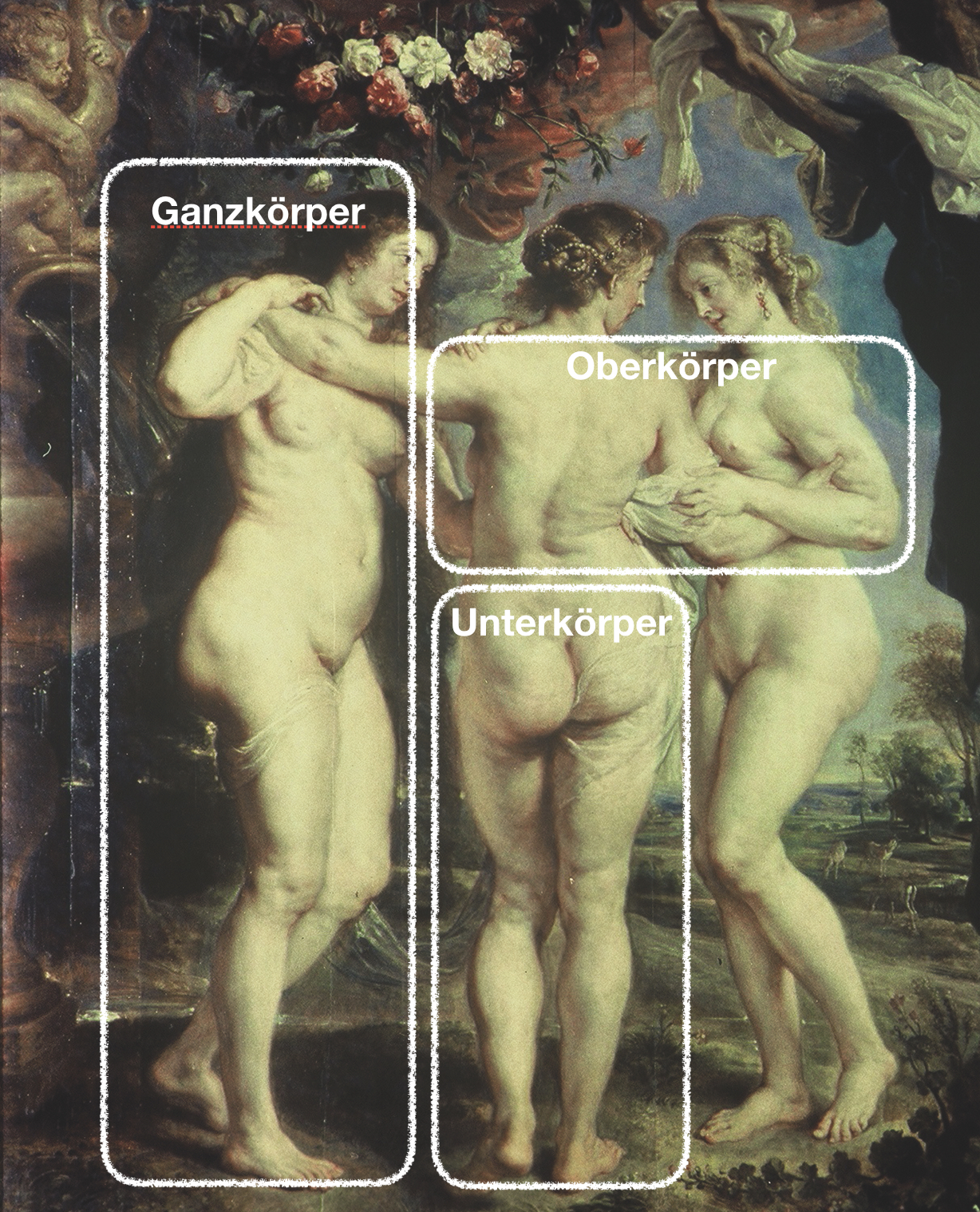
In clinical everyday life it seems to us - if already a further classification - to distinguish between a lower body type and an upper body type.
- Lower body type: This is the "normal", most common course. First there are strong legs, then the weight gain slowly spreads from the bottom to the top. In the end, the swelling may be present everywhere.
- Upper body type: Here the symptomatology starts in the trunk area. Especially the abdomen, back, neck and upper arms increase significantly, while the upper and lower legs remain slim.
- Whole body type: swelling occurs evenly over the entire body and develops without significant disproportion. The distinction from pure obesity is fluid.
Swelling without pain
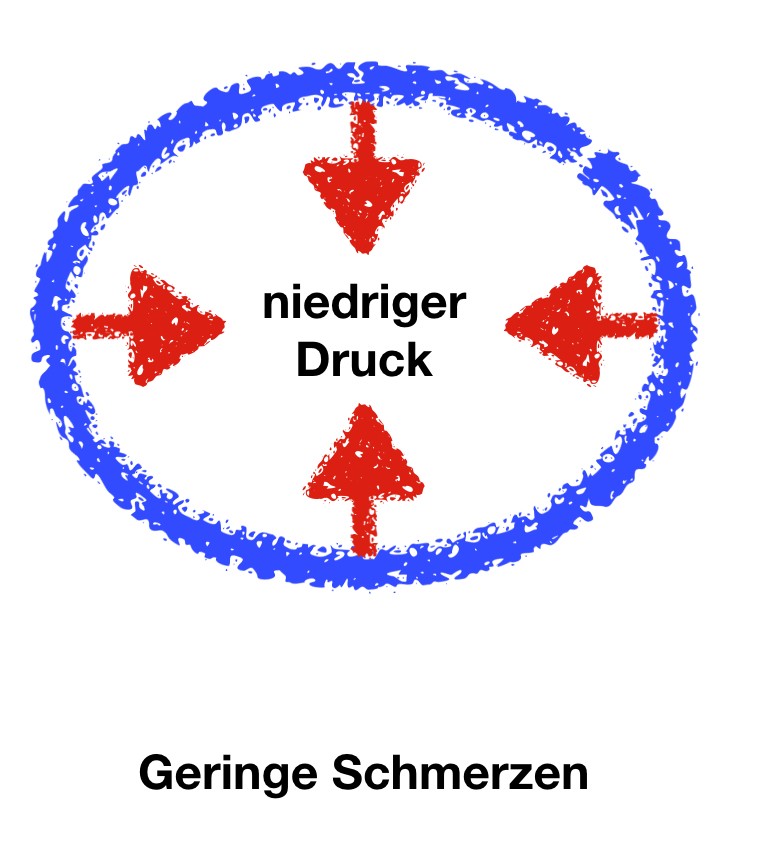
Lipedema is "actually" painful. However, some women have the typical legs as in lipedema and at the same time no pain at all. This is then sometimes referred to as "lipohypertrophy".
It is distinguished from lipedema and called a "constitutional body shape variant".
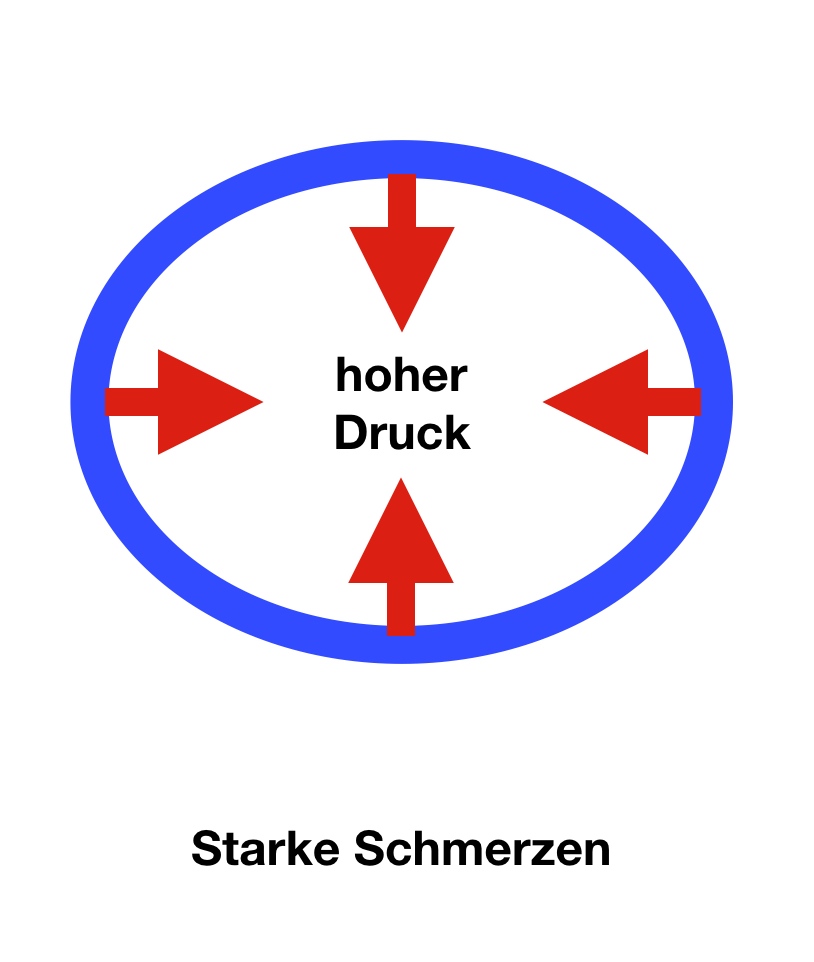
From our point of view, the difference from lipedema is much less sharp. The decisive difference is probably the stability and elasticity of the skin. If the skin tension is high, there will be a high pressure in the inner part of the leg and therefore increased pain.
If, on the other hand, the skin is "super soft", it yields easily and the increase in pressure is very slight. Accordingly, the pain is also less.
We therefore classify this as a subform of lipedema in women with very flexible, soft connective tissue.
Therapeutically, the skin must also be tightened in this constellation - in many cases this can be done without surgery.
By the way: In another field of medicine, lipohypertrophy is also understood as the swelling in the subcutaneous connective tissue that occurs when insulin is repeatedly injected into the same area - e.g., the abdomen.
Pain without swelling
In recent years, we have repeatedly seen slim female patients with pronounced complaints but comparatively slim legs. They suffer from the same complaints as other patients, only hematomas (bruises) are less common in them.
These mostly young women probably also suffer from increased permeability of the smallest vessels. At the same time, however, they have very tight, firm skin. If edema occurs, the skin only yields slightly and the pressure in the tissue increases rapidly. The result is tension complaints, and in some cases even pain at rest. Fortunately, this constellation of complaints can be treated particularly well. As soon as even a small amount of fluid is removed from the legs, the pressure is reduced and there is usually prompt pain relief. Whether the diagnosis "lipedema" really applies in the strict sense in these patients remains to be seen. Much more important is the therapeutic success that can be achieved quickly in these patients.
Causes

One of the most interesting questions concerns the biological background. Is there really a "defect" in the affected women? Do patients with lipedema simply eat too much and, above all, the wrong things? Is it solely due to a lack of exercise? The longer we study the subject, the greater the doubts about such a simple view. Other contexts must at least be considered.
To understand the changes in a deeper way, it is necessary to remember the biological origin of man. We have not always lived in fully air-conditioned offices, but originated from prairie, savannah and jungle. The living conditions of hunter-gatherers shaped our physique and physiological organization. Thus, we are extremely enduring and able to run for hours. This enables us, for example, to hunt animals that are vastly superior to us in terms of short-term top speed. In terms of food, scarcity was the rule and abundance rare. If we were lucky enough to hunt, our ancestors really had plenty to eat with a shot wildebeest. But this luck also had its downsides: There was certainly soon competition in the form of hungry big cats and small fellow eaters - bacteria, worms and insects - which also feasted on the animal. In short, prehistoric humans probably would have given quite a bit for a freezer. Thus, they were forced to quickly absorb the available calories and store them close to the body.
Voluptuous women
Of course, these correlations apply especially to women. During pregnancy and especially during lactation, their caloric needs increase considerably. 200-300 extra kilocalories during pregnancy and 500-700 kcal during lactation were not easy to organize. This may not seem like much. But per pregnancy and breastfeeding time several hundred thousand kcal come together. Converted into fat, that's several kilograms (about between 20-40 kg).
Therefore, our female ancestors prepared themselves for this energy dilemma from puberty on. The result was curves, which at the same time signaled to men: "With this woman, abundance of children is guaranteed". Women with pronounced shapes were therefore at an advantage in several respects: they had supplies to get themselves and their children through bad times, and prehistoric men must also have found the curves highly attractive.
Bad connective tissue?
Almost all women who come to us complain about "bad" connective tissue. What is meant is soft, stretchy tissue, often associated with vein problems. Again, I would like to ask if the tissue is really just "bad" or if there is also something "good" about it.
The collagen fibers of connective tissue are stronger than steel. But during puberty, in girls, they slowly become softer and more stretchable. The advantage is quite obvious: soft tissue provides optimal conditions for a natural birth. Imagine a woman having to give birth to her child under the simplest of conditions and without assistance. In this case, the soft, stretchy tissue offers the very best conditions for a speedy and gentle birth. Women with harder tissue probably also had slender legs in the primeval forest. But this "advantage" carried the risk of not surviving a birth.
Women and men
- Women have a different fat distribution than men. While men tend to accumulate fat on the abdomen ("beer belly"), women store fat much more frequently on the hips, buttocks and thighs.
- The subcutaneous fat layer is twice as thick on the legs of normal-weight women as it is in men.
- The waist-to-hip ratio (waist circumference divided by hip circumference) should thus be less than 0.8 in normal-weight women and between 0.8 and 1.0 in men. If it is higher, then this represents a risk factor for cardiovascular disease. An "apple figure" is therefore much more dangerous than a pear figure. Women are thus naturally favored.
- Fat cells are stabilized by connective tissue in men and women in very different ways. In men, the fibers have a reticular or scissor-grid-like structure, whereas women have significantly larger fat chambers that are oriented perpendicular to the skin surface. They are therefore also referred to as "standing fat chambers".
- Since male skin is significantly thicker than female skin, the so-called pinch test gives a different result in completely healthy women compared to men. The upright fat chambers of a woman are pushed together and thus become visible. This effect is therefore natural to a certain extent and increases with age because the skin becomes somewhat thinner. Thus, the "upright fat chambers" become more easily visible. In men, on the other hand, only a fine folding or furrowing of the epidermis is visible.
Bad vessels?
One of the known causes of lipedema is increased capillary permeability. According to the German guideline, there is a "capillary permeability disorder". But is that the only correct view? A disorder? Here, too, we have doubts. The increased permeability also has advantages: During pregnancy, the transport of nutrients and oxygen is generally increased in women. The unborn child thanks them with strong and healthy growth.
In this respect, the increased permeability of the capillaries can also be an expression of a particularly female form of organization. Only the best for the baby! Of course, there is no light without shadow: edema during pregnancy, increased hematomas (bruises) and increased influx of nutrients into the lower parts of the body are the negative consequences of this positive supply.
Possibly, the increased bleeding readiness with hematomas (bruises) must also be seen in this context.
Problematic protein
All protein that has leaked from the capillaries and the water bound by it can be removed exclusively via the lymphatic system. This works well for quite a while because the lymphatic system has a certain reserve capacity. When more lymph fluid is produced, it can also transport more.
At some point, this capacity is exceeded. A visible swelling, an edema, now develops. If we stand or sit a lot, this edema occurs especially on the legs.
The fluid that flows out of the capillaries also contains fat, mostly in the form of triglycerides. They supply the cells with valuable energy. The more protein and thus water in the tissue, the more fat is stored in the subcutis and is then very difficult to break down again. The path to the subcutaneous fat depots becomes a one-way street. It is easy to get in, but extremely difficult to get out.
The result: an explosive protein-water-fat mixture accumulates in the subcutis. The thicker it gets, the worse lymph transport and fat breakdown become. And the worse these substances are broken down, the more of them accumulate - a vicious circle!
Problematic veins
Now, when the legs increase in circumference, another factor comes into play. The skin loses some of its elasticity and becomes more stretchy. This also has an unfavorable effect on lymph flow and lipedema.
When we stand in one place for a long time, for example, while standing in line at the checkout, blood accumulates in the veins of the legs. The pressure in the veins increases considerably. However, if we walk a few steps or just bob our toes a little, it reduces considerably. We owe this relief effect to the interaction of muscles and the venous valve system. The veins are actually compressed by the muscles. Since they have valves similar to those of the lymphatic system, the muscle movement causes a great deal of blood to be pumped back from the veins to the heart.
The prerequisite for the functioning muscle pump is the elastic pressure of the skin on veins and muscles. The skin acts like a natural compression stocking. Without this compression, venous blood would choose the path of least resistance and escape into the stretchy subcutaneous tissue. Pain and swelling would result.
The overstretched skin in lipedema has exactly this consequence. It no longer acts like a strong compression stocking, and the veins pump fluid into the subcutaneous fat tissue. The edema accumulates in the legs and further overburdens the lymphatic system. Many of those affected are surprised to notice the effect on themselves: After sports, the legs used to be slim, now the swelling even increases after exercise.
Veno-arterial reflex
It's hard to believe, but the arteries also contribute to edema. In healthy people, there is an important protective reflex that limits edema. If the pressure in a vein increases, they give a "command" to the artery that supplies them. This then contracts and the blood flow decreases. As a result, the pressure in the vein also decreases.
In lipedema, this "veno-arterial reflex" is defective. Although the veins are overfilled, the arteries do not stop the blood supply. The veins virtually overflow, and yet the artery still lets blood into the flooded area. Thus, the increase in edema also occurs through this mechanism.
Neurogenic inflammation
Lipedema is an extremely painful condition! Strangely enough, the pain itself leads to an increase in edema. The phenomenon is called "neurogenic inflammation" (= nerve-mediated inflammation) and is well known in pain research. What is meant by this is that permanent overexcitation of nerves leads to inflammation in the pain area. As a result - as with any inflammation - capillaries become more permeable, leading to further swelling and thus further pain!
Progress
Lipedema does not affect life expectancy. However, there is also an unfavorable message: if lipedema is not treated in time and properly, it usually worsens slowly but continuously. This is especially true if adequate therapy is not initiated. In these cases, additional weight gain - especially during periods of stress - usually leads to an almost precipitous deterioration.
The longer the clinical picture persists, the more the tissue hardens and additional lymphedema develops, which is then referred to as "lipo-lymphedema" or "lympho-lymphedema". Such a development must be expected on average after about 17 years. But: Resignation is by no means appropriate. At any time in life (even in retirement!) the symptoms can improve even with therapy.
Diagnosis
Often not diagnosed
Lipedema is rarely diagnosed and often confused with other conditions, especially overweight (obesity) and lymphedema. Often the affected women have years or decades of suffering behind them before the correct diagnosis is made.
Very often, patients are told that they should eat less and exercise more. But that is exactly what most of them have already tried countless times without success. They are therefore often accused of eating on the sly.
As a rule, no complicated examination procedures are needed for a correct diagnosis. A simple survey of the complaints and history as well as a physical examination are usually quite sufficient.
Symmetrical swelling of the legs (and/or arms) is typical, although the backs of the feet and hands are not affected. The swelling is pressure painful, hematomas (bruises) are common. The symptoms usually begin during puberty. Diets are ineffective.
Neither lipedema nor cellulitis can be proven by a specific laboratory test. However, laboratory values help rule out other conditions that also cause edema.
A physician may therefore determine some laboratory values. Here are the most important ones: protein electrophoresis, total protein, sodium, potassium, creatinine, urea, uric acid, creatinine clearance, urine status, transaminases, alkaline phosphatase, bilirubin, T3, T4, TSH, cortisol if necessary.
One important small detail plays a major role in distinguishing lipedema from lymphedema. It is the question of whether or not it is possible to lift the skin over the toes or fingers. In lipedema this is possible, but not in lymphedema, where the swelling also includes the feet or hands. One speaks of a positive (no lifting possible) or negative Stemmer's sign (lifting of the skin possible).
Stemmer's sign
More exact determination
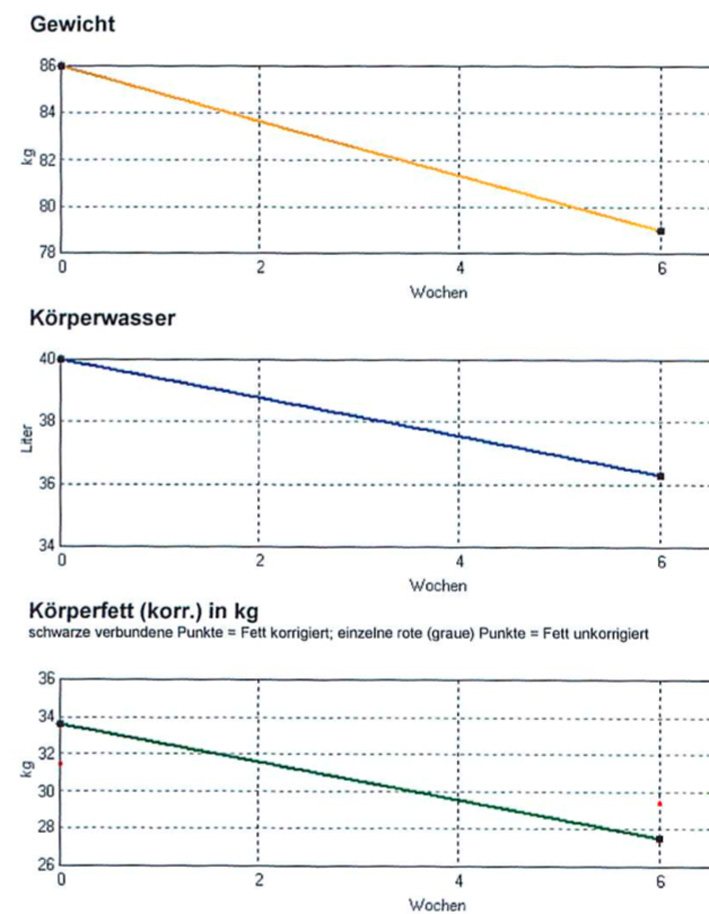
Measuring edema, or water retention, is more difficult than it might seem at first glance. If you stand on a scale, the body is treated as if it were made of a single material. No distinction is made between organs, fat, muscle and water.
In recent years, one often finds scales that additionally display the fat content on the scale. To indicate this value, a harmless, high-frequency alternating current is passed from one leg to the other and the electrical resistance is determined. Fatty tissue, muscles, water, connective tissue, bones and internal organs have slightly different resistance. If these differences can be determined precisely, it is possible to analyze which parts of the body make up the weight.
With simple devices, such as those that can be purchased inexpensively in stores, one can obtain an approximate estimate of the fat values. However, there are devices developed for medical and scientific purposes that allow very reliable examinations. They measure with several frequencies, compare them, correct possible errors and calculate far-reaching analyses from the data obtained.
If you measure several times during the course of a treatment, you can clearly tell whether the therapy is having the desired effect. Fat and water should be reduced, while muscle mass slowly increases at the same time.
Another, simpler method of therapy control is the calculation of leg volume. This involves measuring the circumference of the leg from the ankle to the groin every 4 cm. With the help of a calculation formula, the volume can be determined in this way. In this way, the success of decongestive therapy can be measured in liters. However, it is not possible to distinguish between fat, water and muscle.
Similar, but automated, is a circumference measurement of the legs with the help of a laser beam. Such devices are used, for example, by medical supply stores to measure the optimal compression stockings.
The examination can be supplemented by an ultrasound measurement, which can distinguish between fluid and fatty tissue.
Lymphography, which was frequently ordered in the past, is usually unnecessary. Finally, there are also X-ray examinations (DEXA procedure) for scientific questions, which provide accurate results but are not suitable for daily practice.
Measurement at home
The following measurement method is often used in physiotherapy practices. The highest elevation of the inner ankle is palpated and marked. Then, using a measuring tape, additional marks are placed every 4 cm up to the thigh. At these marks, the circumference is measured as accurately as possible. With the help of a calculation formula or computer, the volume can thus be determined quite accurately.
You can find the automatic calculation sheet below. You can open it with Microsoft Excel orOpenOffice(free of charge).
Form for self-measurement
Diagnosis - Self test
Self-test
Here is a self-test that gives an approximate estimate of whether you suffer from lipedema. Please note that this can of course only give an approximate estimate. The actual diagnosis is made by an experienced physician.
Differential diagnosis - When not lipedema?
Here are the differences between lipedema, so-called lipohypertrophy (see note), obesity and lymphedema. According to the S1 guideline.
| Lipedema | Lipohypertr. | Obesity | Lymphedema | |
|---|---|---|---|---|
| Fat proliferation | +++ | +++ | +++ | (+) |
| Disproportion | +++ | +++ | (+) | + |
| Edema | +++ | ø | ø | +++ |
| Pressure pain | +++ | ø | ø | ø |
| Blue spots | +++ | (+) | ø | ø |
Phleboedema is edema caused by the venous system. Damage to the venous valves and veins increases the pressure in the capillaries. This results in increased fluid formation in the capillaries and connective tissue as well.
Unlike lymphedema, however, this edema is low in protein.
These edemas also differ in their external appearance, usually being deeply depressible, i.e. forming dimples, in contrast to lipedema. Finally, there is often a bluish discoloration of the skin. However, there are transitions between lymphedema and phlebedema if inflammation additionally damages the lymphatic channels.
In the course of prolonged venous insufficiency, the skin on the lower leg often turns brownish and local inflammation or "open legs" (ulcus cruris) may occur.
Edema due to heart failure
Often, women with "thick legs" fear they may be suffering from heart disease. In fact, heart failure is the most common cause of edema, especially in older people. However, these water deposits are of a completely different nature than in lipedema. They are position-dependent, symmetrical edemas. In the evening, the lower legs are severely swollen. They leave behind deeply depressible, painless dents. In addition, there are the typical signs of cardiac insufficiency with shortness of breath on exertion, increased nocturnal urination and other symptoms more. In contrast to lymphedema and lipedema, diuretics (diuretic drugs) are effective and useful here.
Orthostatic edema
Orthostatic edema is the "normal" swelling experienced by many people, especially women, who have to sit or stand for long periods of time. Saleswomen, flight attendants or other professions that require being on their feet for long periods of time are often affected.
This type of swelling occurs mainly in the evening and is gone the next morning. On vacation, it is absent altogether, unless you have to stand all the time. - No reason to worry! Nevertheless, lighter compression stockings can be helpful.
Idiopathic edema
Very many women know these complaints: Especially in the second half of the cycle, they wake up in the morning with puffy eyes, almost as if they had looked too deeply into the glass in the evening. The rings stick to their fingers, their breasts tighten and the scales show a considerable increase in weight, although they have not eaten more than usual. It is true that the swellings on the face and hand get better in the course of the day. But by the evening, the legs are tense. In addition, they feel fatigued, dull and irritable.
The increased water retention in otherwise healthy women has many names. Since it occurs mainly in the second half of the cycle, i.e. after ovulation, it is often referred to as cyclic idiopathic edema. The word "cyclic" is self-explanatory, since the symptomatology occurs completely regularly. Some women suffer only in the days immediately preceding their period, while others can distinguish two good weeks from two bad weeks. In medicine, "idiopathic" refers to clinical pictures whose cause is unknown.
More familiar is the term "premenstrual syndrome", i.e. a pattern of symptoms that occurs primarily before (pre = before) menstruation, the period bleeding.
However, the same water retention can also occur largely independently of the period and, for example, only increase during warm, humid weather. In summary and more neutrally, these symptoms can therefore be referred to as fluid retention syndrome (retention = restraint).
Paradox: Edema due to medication

Whenever you regularly take medication, it is worth taking a look at the package insert. Can they cause water retention (edema)? Strangely enough, diuretics can also cause edema!
In case of lymphedema and also in case of lipedema these preparations should not be given. This is because when they are taken, there is a loss of water and salt, which the body tries to prevent by producing a hormone. This hormone (aldosterone) remains elevated even if the diuretic tablets are no longer taken or are taken slightly less.
The result: increased water retention. Those affected can no longer get off the tablets!
Madelung disease
Madelung's disease ("Madelung's disease") is a veryrare fatty tissue swelling, mainly in men, that occurs in the neck and shoulder area. The non-encapsulated fatty tissue swellings limit the mobility of the head and do not respond to any diets. Affected individuals are often very lean in other areas. Surgery is often appropriate here.
Lipedema and fibromyalgia
(copy 16)
Therapy: Avoid ineffective!
Frustrating previous experiences
Most women have had extremely frustrating experiences with various therapies. Diets have shown - if at all - at most a short-term success. Shortly after the starvation diets, the pounds are back on the hips. Sweatyspinningin the gym tends to increase the pain. Compression stockings pinch and therefore often lie in the closet. Manual lymphatic drainage is wonderfully pleasant, relieves the pain of congestion, but unfortunately only works for a short time. The happiness often lasts only for a day, sometimes only hours. And after two or three prescriptions, the family doctor will point out budget problems.
Avoid ineffective
In general, little or nothing can be achieved even with drug therapy. In particular,diuretic drugs are out of place.
Lipedema also resists all efforts in thefitness studio. Although physical fitness increases and muscles grow, lipedema is almost completely unimpressed by this.
Many sufferers have wide experience with remedies and remedies without effect. Drugs, especially water-pushing agents, can even do harm. In particular creams, ointments and other preparations to be applied externally are ineffective. The magazine "Öko-Test" succinctly stated after an investigation: "These means do not work" (issue 5/04) - meaning the expensive creams of various cosmetic manufacturers. In an eight-week study, the testers documented "no effect at all worth seeing" in 12 of 19 products. In other words: Poor.
Surprisingly also most parliamentaryallowance are ineffective. That is for many concerning hardly to understand. Why should a Lipödem not be to be eliminated by weight reduction, since it became nevertheless clearly worse in the context of the weight increase?
In fact, however, this is not possible! Affected women usually complain that they lose weight extremely badly and if they do, it is in the wrong place. Those affected lose weight very slowly, but of all places, not where they didn't want to! So often the upper body becomes slimmer but legs and hips remain as they were. This is the opposite of what should be aimed for. The background is probably the congestion in the fatty tissue. As long as the tissue is swollen, the fat there will not be removed even during a starvation diet.
And what aboutmanual lymphatic drainage? It is undoubtedly effective, as can be seen immediately after the therapy. But even 2,3 or more prescriptions of 6 applications each, the legs are by no means much better.
About sport
"In itself" correct and yet ineffective!
"By themselves", of course, exercise, diet and also manual lymphatic drainage are useful and correct. But why don't they help?
Diets: From our point of view, there are two problems here:
- Lipedema is a protein-based edema. Diets with a strong emphasis on animal protein seem to us to be unfavorable, because here at least the breakdown of the excess stores in the area of lipedema is not promoted. Therefore, we prefer diets with little animal protein and, of course, little fat.
- The access of the body is limited for the stagnated area. It can much more easily fall back on the regions with normal blood supply. Therefore, sufferers become slim where they are already slim.
Exercise: If the tissue and especially the legs are severely swollen, the drainage from the smallest veins and lymphatic vessels is impeded. Typical is the increase of pain and swelling after sports. Those who nevertheless pull themselves together and simply continue to exercise often experience a slow increase in the circumference of the legs despite (actually "because of") the sport. Therefore, sports should only be done with sufficient compression (usually compression tights) and only when the legs are already
sufficiently decongested. Otherwise, of course, exercise remains in the water.
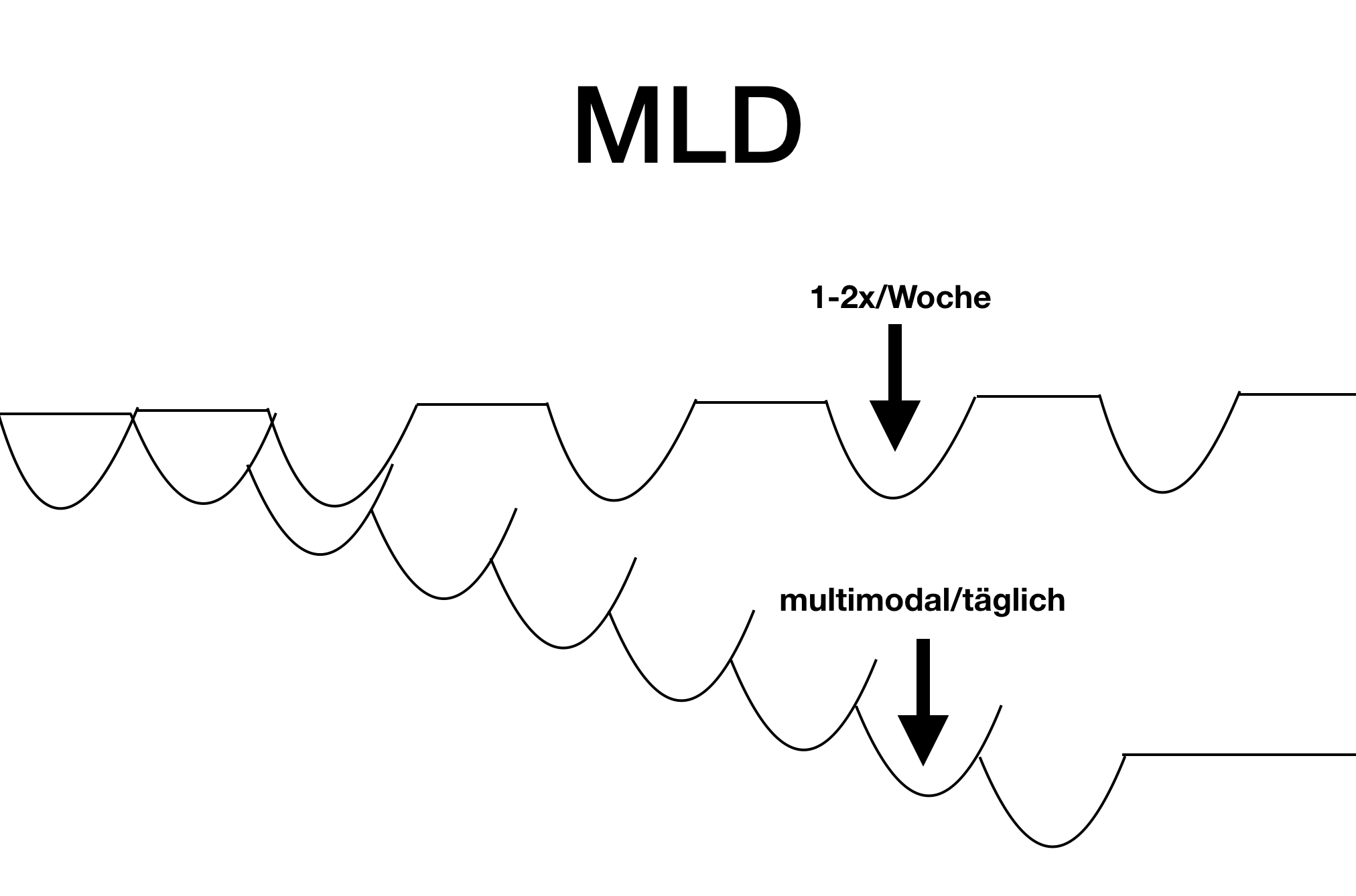
Manual lymphatic drainage: This is quite a wonderful procedure, but it is usually incorrectly dosed. MLD once or twice a week only results in relief for that day - and sometimes only for a few hours. It's like starting over every time, or like taking your blood pressure pills only ever on Mondays.
High protein diet
Many patients often turn to a "low carb" diet on recommendation and eat a very high protein diet. In our experience, this is unfortunately often not successful. Especially in women who suffer strongly from feelings of tension in the legs or body, this - after short-term weight loss - does not lead to significant improvement.
Operations - liposuction?
Surgery, usually liposuction, is not naturally ineffective. However, it also has side effects that must be carefully weighed. The experiences that patients report to us with surgery are to a greater extent problematic. However, it is possible (it is even probable) that all highly satisfied patients do not come to us. Therefore, we mainly see patients who have not had a good experience with the surgical procedure.
These are mostly the following experiences:
- Complications, e.g. infections after the operation
- Lymphedema after the operation
- Unsatisfactory aesthetic results
- Weight gain in the non-operated parts of the body.
Especially the weight gain in other parts of the body very we frequent. For example, the legs were operated but after some time (a few months to 1-2 years) there is weight gain in the abdomen, arms and back.
Therefore, we are quite cautious about surgery, since it is usually possible to achieve good results with the procedures presented here, with which the affected persons are very satisfied.
However, surgery can make sense in certain (rare) constellations. However, conservative (i.e. non-surgical) procedures should have been exhausted beforehand. As described above, lymphatic drainage once or twice a week plus compression stockings are not sufficient in the vast majority of cases. However, this does not mean that conservative methods are ineffective. It depends - as so often - on the right dosage.
Therapy: Use effective!
The basic rules for success
Lipedema is really not easy to treat. The success of individual therapy methods is indeed usually modest. But there is a recipe for success that is as simple as it is effective. It's called: make do, don't spill the beans!
Used sensibly in combination, supposedly "ineffective" procedures suddenly turn out to be very effective. Suddenly, within a few weeks, a change takes place that was previously impossible in months. And these are the principles of an effective treatment, usually referred to as "multimodal therapy":
- A single decongestive procedure is not enough. Several therapeutic approaches must be combined.
- Passive procedures (massages, lymphatic drainage) need active therapies as a supplement (swimming, muscle building, walking with compression).
- No therapy without dietary changes and weight reduction!
- Low frequency treatments are not sufficient if the body is in a state of congestion. 14 therapy days at a stretch are much more effective than one treatment day per week for 14 weeks.
Targets
- Improvement of the disturbed microcirculation
- Reduction of excessive protein leakage from blood vessels Increased removal of protein and fluid
- Reduction of subcutaneous fat
- Strengthening of the connective tissue
- Reduction of excess weight
- Smoothing of skin contours
- Reduction of stress
The following is a list of therapy modules that have proven successful in treatment.
Compression method
Certainly, compression procedures take the first place among all therapeutic procedures. By increasing the pressure on the legs (rarely arms), the return flow from veins and lymph vessels is significantly increased. If you wear compression stockings or put on a bandage, 50% more fluid flows back out of your legs even at rest.
The advantage is even more pronounced during exercise. Without the increased pressure from outside, the muscles would not pump the fluid towards the heart but also into the subcutaneous fatty tissue of the legs, since they lack an appropriate support.
How does this positive effect come about through a fairly simple therapy? When pressure is applied to the leg from the outside, it spreads evenly inside the legs. Muscles, tendons, bones, connective tissue cannot be compressed. They behave like water, which cannot be compressed. On the other hand, blood and lymphatic vessels do. Thus, the entire pressure is directly applied to the vessels.
Blood and lymph follow the path of least resistance. Since the subcutaneous fatty tissue is now compressed, you can not help but flow towards the center of the body. The legs are relieved.
However, compression is only effective if it is done correctly. The pressure in the legs naturally increases towards the feet. Therefore, the pressure of compression should be greater at the ankles than at the thighs, otherwise blood and lymph would accumulate there.
This is where physics comes to the rescue. The effect of a bandage or compression stocking depends on two factors. On the tension and the diameter. The smaller the diameter, the more force is applied to the leg. Everyone knows this from a rubber ring. If you take two rubber rings of equal strength with different diameters, the smaller one is much harder to stretch than the larger one.
Since the ankle is the thinnest part of the leg, the greatest pressure automatically builds up here, while the thigh is compressed the least. In this way, the blood flow is directed in the right direction.
Problems arise, however, if the lower legs are very bulky. Then a compression stocking must be worked much tighter. The manufacturers of the stockings also pay close attention to this relationship between diameter and pressure curve.
Compression bandages
Compression bandages are even more individual than custom-made compression stockings. In this case, a sophisticated technique with a series of bandages as well as padding material is used to achieve an optimal fitting for the momentary situation.
First, the skin of the legs is cared for, wrapped with a tubular bandage, extensively padded, and then gradually compressed with 20 or more bandages. In some cases, the compression is further reinforced by compression tights, e.g. on the hips ("Bermudas").
As for the bandages, short-stretch and medium-stretch bandages are used. These are low-stretch bandages that again combine low resting pressure with high working pressure. The bandages should be worn between 22 and 23 hours a day.
It should not be concealed that compression bandages are used almost exclusively in the hospital. In the "decongestion phase", this reduces edema. Later, in the "maintenance phase", patients usually wear compression stockings.
However, there are patients who learn the bandage technique in a course. At home, they are then able to help themselves excellently. This training is necessary because incorrect compression has the opposite effect. Incorrectly applied bandages abrade and thus worsen the edema.
Compression stockings
So if compression has so many benefits, then all affected women should be happy to wear compression stockings. But that is by no means the case! When I bring up the subject in the consultation, many women bat their eyes at the ceiling. "Yes, I have something like that somewhere in my closet. But you can't wear it, certainly not in the summer."
There is one fundamental problem that cannot be solved. Because of their low stretch, compression stockings simply don't put on well. However, there are aids with which even older people can manage to get into the stockings without undue effort. It depends on the right advice and the selection of the optimal compression stockings. Only then can one become comfortable with this therapeutic aid.
It is important to put on these stockings already in the morning, when the legs are not yet swollen. This is especially true on days when long periods of standing are unavoidable. There are many types of compression stockings. There are two methods of manufacturing: circular knitted and flat knitted compression stockings in different compression classes.
Apparent compression
In the search for other methods of compression treatment that would be easy to perform, devices for fully automatic therapy were developed.
In principle, this treatment involves placing a cuff around arms or legs. They look like oversized sleeves or pants. They contain air chambers that are rhythmically inflated by a compressor.
Initially, people tried single-chamber systems, but soon found out that it is not a good idea to apply pressure evenly to the leg. As with compression stockings, the pressure must be higher at the ankles than at the thigh. This is the only way to improve fluid flow in veins and lymph vessels.
Manual lymphatic drainage
Lymphatic vessels can actively contract. The opening and closing of the valves in the lymphatic vessels thus results in the onward transport of waste products. At the same time, the lymph flow is stimulated by muscle activity, similar to the veins.
In manual lymphatic drainage, this natural process is supported by a special massage. Through a skillful technique, a mixture of pressure and suction is applied to the congested tissue. In this way, physiotherapists ensure an increase in lymph flow. They use grip techniques whose names, such as "pump grip" or "scoop grip," already explain their function.
In this way, the lymph vessels' own movement is stimulated and the fluid is shifted toward the center by gentle pressure. If the pressure on the skin is released, a negative pressure is created with the help of the flap action, which sucks in the lymph fluid from below. These light movements are made rhythmically approximately every second, massaging each area of skin 5-6 times in succession.
If the legs are successfully decongested by manual lymphatic drainage, then compression should be performed immediately afterwards, i.e. compression stockings should be worn or a bandage applied.
In case of pronounced complaints, the massage is performed in clinics up to twice a day. In between, the legs are fitted with compression bandages. The combination of the two procedures are the essential components of the so-called complex physical decongestion (CPD), with which lipedema is treated in an inpatient setting.
Manual lymphatic drainage is an exceptionally successful method of treating lymphedema. In the case of lipedema, the results are not quite as good. In addition, the massages should be performed as frequently as possible, otherwise the effect wears off after a very short time.
Unfortunately, such frequent frequency is not possible in most cases for reasons of cost and time. Nevertheless, those who suffer from lipedema should try to enjoy this beneficial therapy at least from time to time.
Vacuum method
Instead of exerting pressure on the tissue and thus promoting reflux, there is also the reverse approach of sucking out the edema with negative pressure. This idea is also pursued in lymphatic drainage, which uses pumping and scooping movements to draw the lymph fluid out of deeper regions.
The oldest and best-known way of using negative pressure therapeutically is cupping. Here, the air in a glass is heated for a short time by a flame and placed firmly on the skin, e.g. on the back. While the air contracts as it cools, a vacuum is created in the glass, which exerts a powerful negative pressure on the tissue. The skin now bulges out, there is redness and slight swelling below the cupping glass.
For thousands of years, this procedure has been used primarily to treat muscle pain. Independent of a possible influence on the lymph flow, skin stimulation occurs, which is supposed to contribute to pain reduction. Instead of a classic cupping glass, there are also glasses with an attached rubber ball. In this way, a negative pressure can be created without the cumbersome heating of air.
Unfortunately, classic cupping is unsuitable for the treatment of lipedema and cellulitis, since the pressure is limited exclusively to a very small area and, in the best case, the edema is displaced.
Cupping massage
A variant of cupping is cupping massage. Again, cupping glasses are used. In preparation, the skin is oiled. Then the cupping glass is pulled over the skin with negative pressure. The direction of movement should mainly follow the lymph flow, i.e. from the feet towards the upper part of the body.
Initially, we advised our patients to be very careful and cautious, otherwise there is a risk of hematomas (bruises). This is especially recommended if the legs are very swollen and therefore sensitive to pain. However, some of our patients did not follow this advice and performed the negative pressure massage very vigorously.
As expected, the feared side effects occurred. However, something else became apparent: after a few weeks, the tissue tightened and the skin became smoother and more beautiful. Could it be that damage, of all things, leads to improvement? This is certainly conceivable, since stretching stimuli to the limit of the injury simultaneously trigger regeneration and growth stimuli that give rise to more stable and functional tissue. This may even lead to the activation of stem cells in the connective tissue. In cosmetics, cupping massages and similar techniques have therefore long been used to tighten tissue.
We have developed an app for self-help.
Endermology (LPG)
Another massage technique is endermology. Here, a skin fold is captured, rolled in and out with a device specially developed for this purpose, and thus a kind of "skin gymnastics" builds up the connective tissue. Not only the skin but also the underlying connective tissue is captured and also the subcutaneous fat deposits.
Movement
For patients with lipedema, exercise is vital. However, only under one condition - compression stockings must be worn!
Without compression, there is a risk that the muscles, blood and lymph will not pump to the heart but into the tissues and under the skin. The swelling then increases significantly after movement, and sport becomes a frustrating experience.
For patients with lipedema, endurance sports that strengthen the legs and hips have proven especially effective. For many women, walking or Nordic walking is an excellent sport. Not least because it puts little strain on the joints, is easy to learn, can be done anywhere and is effective. Moreover, Nordic walking even trains the arms. There are many courses where this sport is taught. In the beginning it is a bit unusual to walk with poles through the forest, but this will soon pass.
Of course, cycling or training on the exercise bike is also an excellent form of exercise for the legs and pomus muscles. For those who have no inhibitions about the swimming pool, regular swimming, aqua jogging or other forms of exercise in the water are highly recommended. Here compression stockings are superfluous, because the water pressure provides natural compression. Many women know from their own experience how effective the combination of exercise and massage by the water is. After a short stay in the water, so much edema is mobilized that they have to get out of the water to go to a quiet place.
Movement in water
Movement in water is a virtually optimal therapy method. First of all, it is possible in a natural way to move lightly, almost weightlessly, in water. Even those who don't do sports or are overweight can perform at least simple movements in the cool water. It is not important to do dozens of lanes in perfect style. It is quite sufficient to move forward "somehow". This alone provides greater strength, endurance and flexibility in the long run. The second advantage of aqua fitness is even more important: the water exerts a powerful but steady pressure on the body. This force acts on the protein-rich edema of the connective tissue. Fluid is shifted from the connective tissue into the blood vessels. The congested veins are also relieved by the water pressure. There is an increase in blood volume around the heart, which is registered by the pressure receptors in the right atrium. They then prompt the kidneys to increase excretion (so-called Gauer-Henry reflex). It does not take long for the urge to urinate to appear. In short: a perfect lymphatic drainage!
You don't necessarily have to go to the swimming pool to exercise in the water! Be creative!
Cold training
In addition to the above-mentioned procedures, countless other treatment methods are also used to treat lipedema and cellulite. The "physical procedures" are mainly based on heat and cold applications. The aim is to stimulate blood circulation and thus promote the removal of lymph and fat. There is a rational reason for this in lipedema. Blood circulation is restricted here, which is often manifested by noticeably cool skin over the swollen areas.
However, all physical procedures are supportive methods. They should be used in combination with compression, exercise and dietary changes.
Swelling increases with heat and decreases with cold. Therefore, we like to expose patients with lipedema to extreme, dry cold to give the vessels maximum incentive to contract. It is a vascular training of a special kind. At the same time, this therapy method effectively counteracts the pain in the deep tissues.
The chamber is pleasantly lit and connected by a large heated window (no fogging) with the anteroom, where the control staff is located. The cold chamber is extremely dry, humidity is practically non-existent. As a result, the low temperature is usually considered comfortable.
One enters the room individually in bathing clothes/underwear and with bathing shoes. If a patient is very prone to freezing, gloves, earmuffs and mouth guards (available from us) can be worn, as well as stockings. The duration of the stay is one to four minutes. During the stay, one should move slowly back and forth in the chamber.
Nutrition
For patients with lipedema, cellulite or water retention, a change in diet is recommended that is gentle on the gastrointestinal tract, effectively reduces weight and also avoids the dreaded yo-yo effect.
Such a change consists of a nutritional structure, which proceeds in several stages. Initially, the gastrointestinal tract is spared and relieved. Similar to the classic diet of porridge or oatmeal, the diet consists mainly of soup or porridge. Subsequently, the diet is built up over the course of several weeks. This phase can be compared to a slow build-up of physical training - jogging for the intestines, as it were. Gradually, more and more fresh and coarser foods are added until a very healthy diet is reached in the final stage. This corresponds to a wholefood or Mediterranean diet. It is essential that sugar and meat are consumed only very moderately, while fruit, vegetables, salad and whole grain products predominate. How the practical structure takes place is described in detail in the last book.
Intensive Therapy
Many patients try in vain for years to fight the pain and swelling. The therapy described above is "actually" simple. In essence, it consists mainly of a consistent change in diet and very intensive decongestion.
The problem with decongestion is that the swelling constantly returns. The success of manual lymphatic drainage (MLD) may last only a few hours, then pain and swelling return. This is not a useful way to treat lipedema.
The standard measures of MLD and compression stockings are "basically" correct, but in most cases they are insufficient. Paradoxically, too much (!) MLD is even used overall, since the treatments often take place over years, but in the wrong dosage!
Make do instead of spill
The main problem of pronounced lipedema is that the created swelling hinders the lymphatic drainage itself. It is similar to a traffic jam on the highway. Breaking up this traffic jam is the real goal of therapy.
So, instead of going to lymphatic drainage once a week for months or years, which is largely pointless, intensive daily treatment for several hours is needed for a limited time (1-3 weeks). A variety of methods are used as part of this therapy (see effective measures).
Above all, these are:
- MLD
- Apparative compression
- Cold chamber
- Vacuum method
- Wrapping
- Endermology
- Exercise
- Change of diet
This is undoubtedly extensive and time-consuming. But in the end, these are fewer applications in total than would otherwise add up over years. In the videos you will find numerous examples of intensive therapy. Please also pay attention to the notes on the videos.
Self-help
Self help at home
In many cases, it is possible to improve lipedema all by yourself at home without extensive therapy procedures. But this requires three things.
- At least two weeks of time
- Sufficient willpower and stamina
- A clear program
You will find the program in a book that not only explains what lipedema is, but also what you can do yourself without outside help.
Be creative!
Exercise in water does not always have to mean "swimming pool". A rain barrel or a wine barrel can also serve well.
Even a child's swimming pool can be used very creatively. (I thank the reader for taking the pictures!).
New: App
We are very pleased that after very long preparation our lipedema self-help APP is ready for use. Here you will find many suggestions for your self-help at home. Especially the systematic decongestion by means of cupping techniques is explained and demonstrated in detail. You will also find films 1:1 to follow along. I.e. you watch the films and simply join in.
The use of the apps is completely free of charge in the current state of development. For formal legal reasons (liability law), we may only activate the apps for patients who are undergoing treatment with us or for whom we have conducted a video consultation. Avideo consultationis fully covered by private and statutory health insurance in Germany. You can book this online.
Videos
First of all, we would like to thank all those affected once again for having the courage to speak publicly about their complaints. We ask you to be respectful of this openness.
It is important to note: These are individual examples from one patient. These films do not represent a general statement about the success of a method in general. Above all, they are not a "promise" or "guarantee" that a particular method is effective in every individual case.
Notes on all films.
Small video tutorial
After one to three weeks of intensive therapy
After several months
Operation?
The experiences that patients report to us with surgeries are to a greater extent problematic. However, it may well be (it is even probable) that all highly satisfied sufferers do not come to us. Therefore, you should keep this in mind when you watch the following videos.
High protein diet?
Lipedema and fibromyalgia/pain
Lipedema is usually associated with pain. But sometimes this pain is so prominent that there is an overlap with, for example,fibromyalgia syndrome or other pain disorders.
Here, it is then of decisive importance for the treatment whether the pain is primarily caused by the edema or originates from other sources. If the edema is decisive, rapid progress will be made as soon as it subsides.