The discomfort is difficult to put into words. The world seems somehow strange and unreal. It is a feeling like fog in the brain or like standing behind a pane of glass. Everything seems unfamiliar, not real or as if in a dream.
And even one's own body is different from what it was. Foreign, like a robot. Looking in the mirror has lost its naturalness.
The whole thing is frightening. A tumor or a nervous disease? Or even an impending mental illness?
Depersonalization and derealization are the names of this phenomenon. What is it? How does it develop? What helps against it? We have new insights into this!
New insights and new understanding
It rarely comes alone
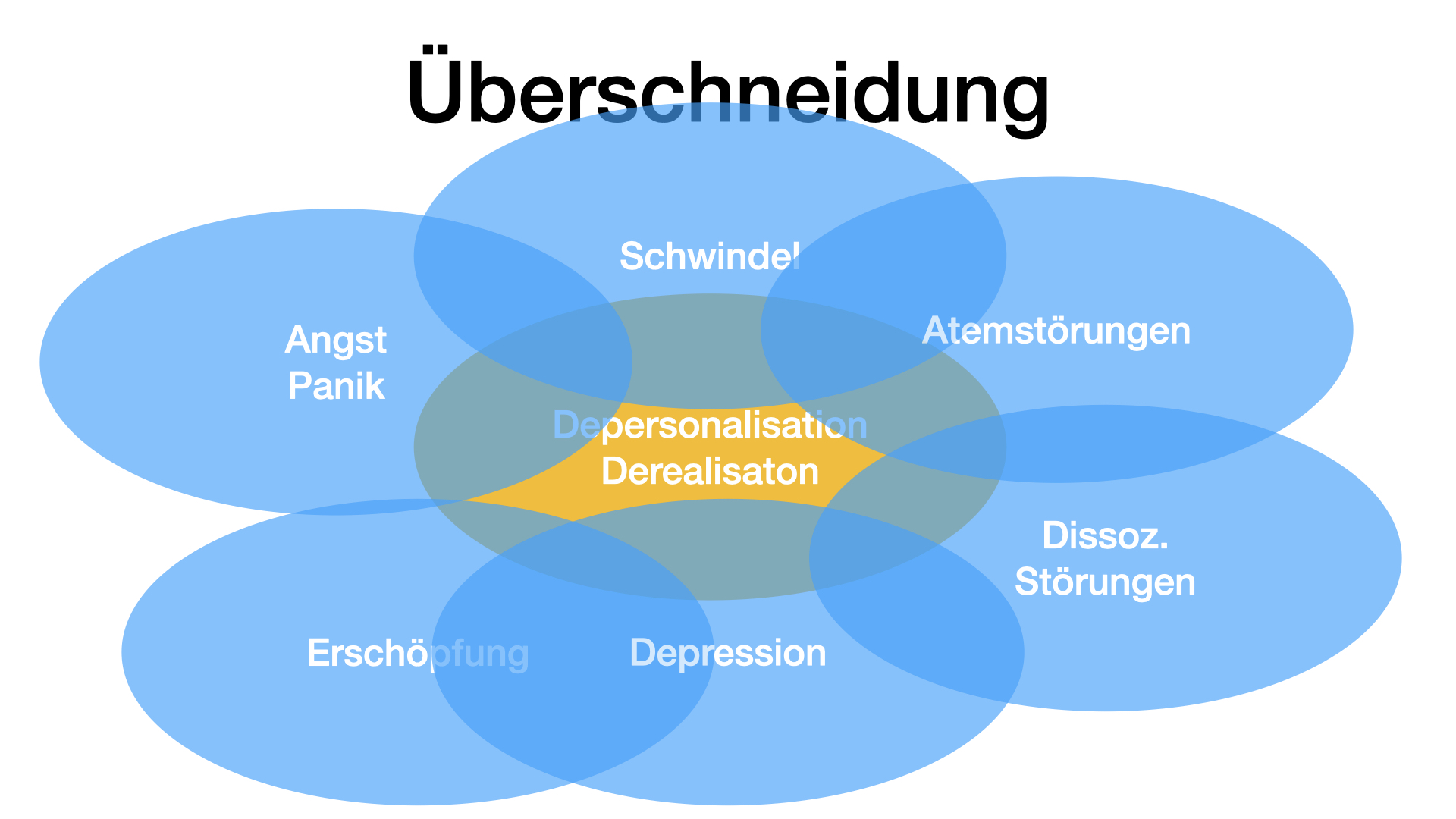
Depersonalization and derealization can be considered as isolated phenomena. However, it is well known that the symptomatology rarely occurs alone. Patients with derealization and depersonalization usually complain of many other symptoms. Most notably, dizziness, fatigue, "fog in the brain," panic attacks or feelings of panic, pain, anxiety, or depression.
Also vice versa
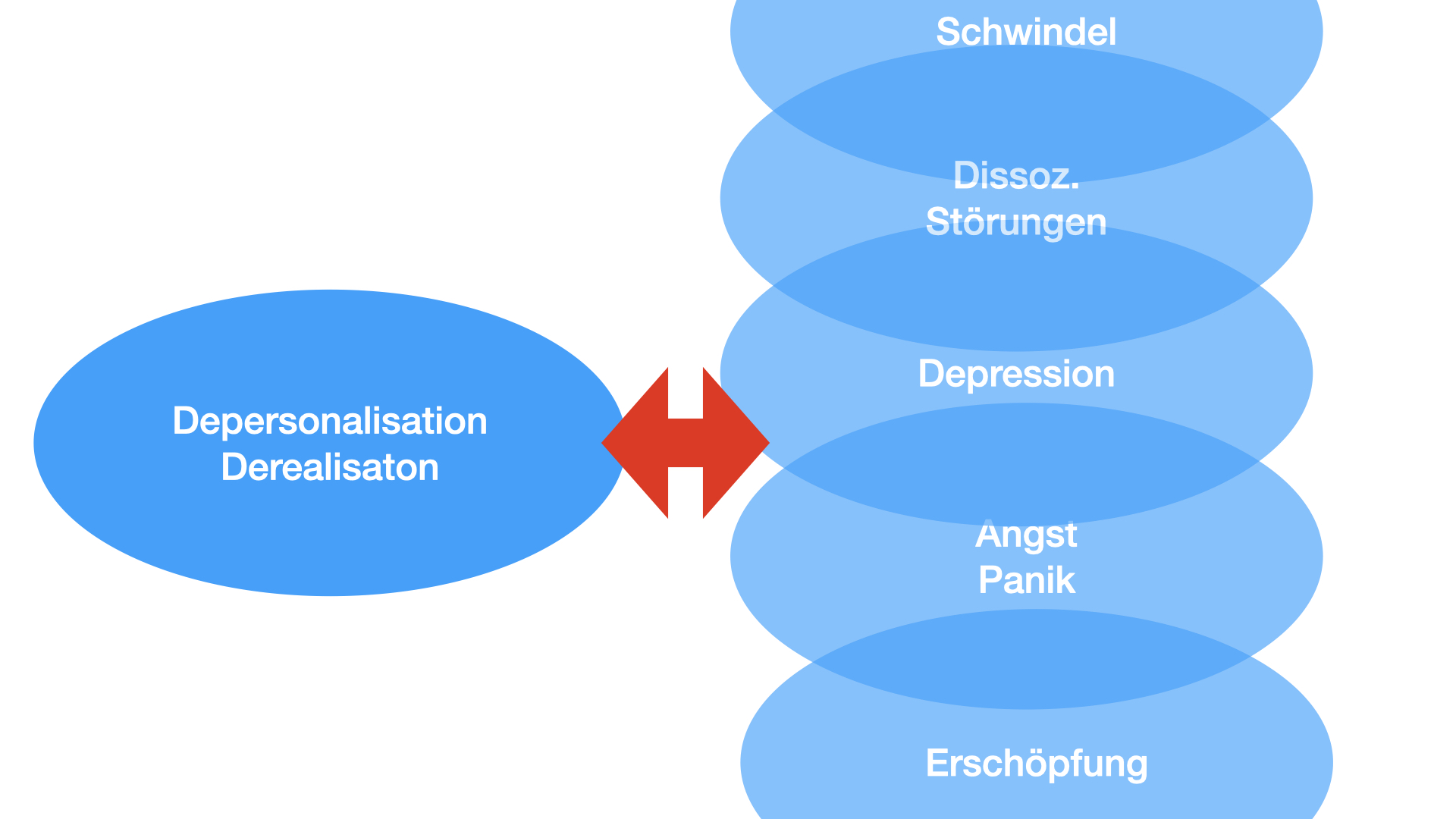
The consideration can also be turned around.
- Patients with functional dizziness usually complain of very pronounced drowsiness, a feeling of being in a fog or of being drunk.
- Patients with CFS or other fatigue syndromes complained of "brain-fog" i.e. a foggy brain.
- Fibromyalgia patients describe massive exhaustion and likewise the feeling of being "beside oneself".
- We see this particularly pronounced in people after a panic attack. Afterwards they are often like "not really there" for a long time.
Even if dizziness, exhaustion, pain, panic or derealization are clearly distinguishable complaints, there is obviously an inner connection that has been little noticed so far.
In clinical pictures such as functionaldizziness,exhaustion,panic disorder, brain fog, CFS and also in some dissociative disorders, we were able to establish a close relationship to breathing disorders. The details can be found in the respective clinical pictures.
Is it conceivable that there is also a connection to disordered breathing in derealization and depersonalization? As believe, yes!
Central to this consideration is the physiological connection of respiration to vascular control of the cerebral vessels. In short, a drop in carbon dioxide levels leads to reduced blood flow to the brain.
Respiration and cerebral blood flow
This restricted supply first affects the higher abilities of the brain: rational thinking, memory, alertness, inner presence, etc.
However, restricted blood supply can also lead to regional disorders, for example in the regulation of balance or in the visual center. The consequences are then dizziness or visual disturbances.
New findings and therapy
Introduction
Symptoms
Symptoms
The complaints were first described in detail in the 19th century. In the , foreground was already then the feeling of alienation often coupled with exhaustion, anxiety and depression.
Derealization
The feelings of alienation are directed at the world, which no longer seems real. It seems strange, unreal, as if through a veil or a fog. Sometimes this kind of perception is described like "a dream", as if the outside world did not really exist or was enchanted.
Depersonalization
Even one's own person seems unfamiliar. Looking in the mirror is no longer natural. One's own hands no longer seem to belong to oneself. The inside seems empty, hollowed out, robotic or as if dead.
Definition
Definition
Currently, there are two definitions of derealization and depersonalization. In theICD it is counted among rare forms of "other neurotic disorders" and in theDSM V it is subsumed under "dissociative disorders".
The following distinction is very important: In derealization the world appearsas ifitwerenot real. In psychosis, the person is convinced the world is changed.
In depersonalization, the world appears as if Iwere looking through someone else's eyes,as if the image in the mirror did not fit me, andas ifmy hands did not fit me. However, I know that this is just how it appears.
In psychosis, my handsare controlled by a stranger, a stranger uses my eyes, my sensations are manipulated from the outside, and so on.
Forms
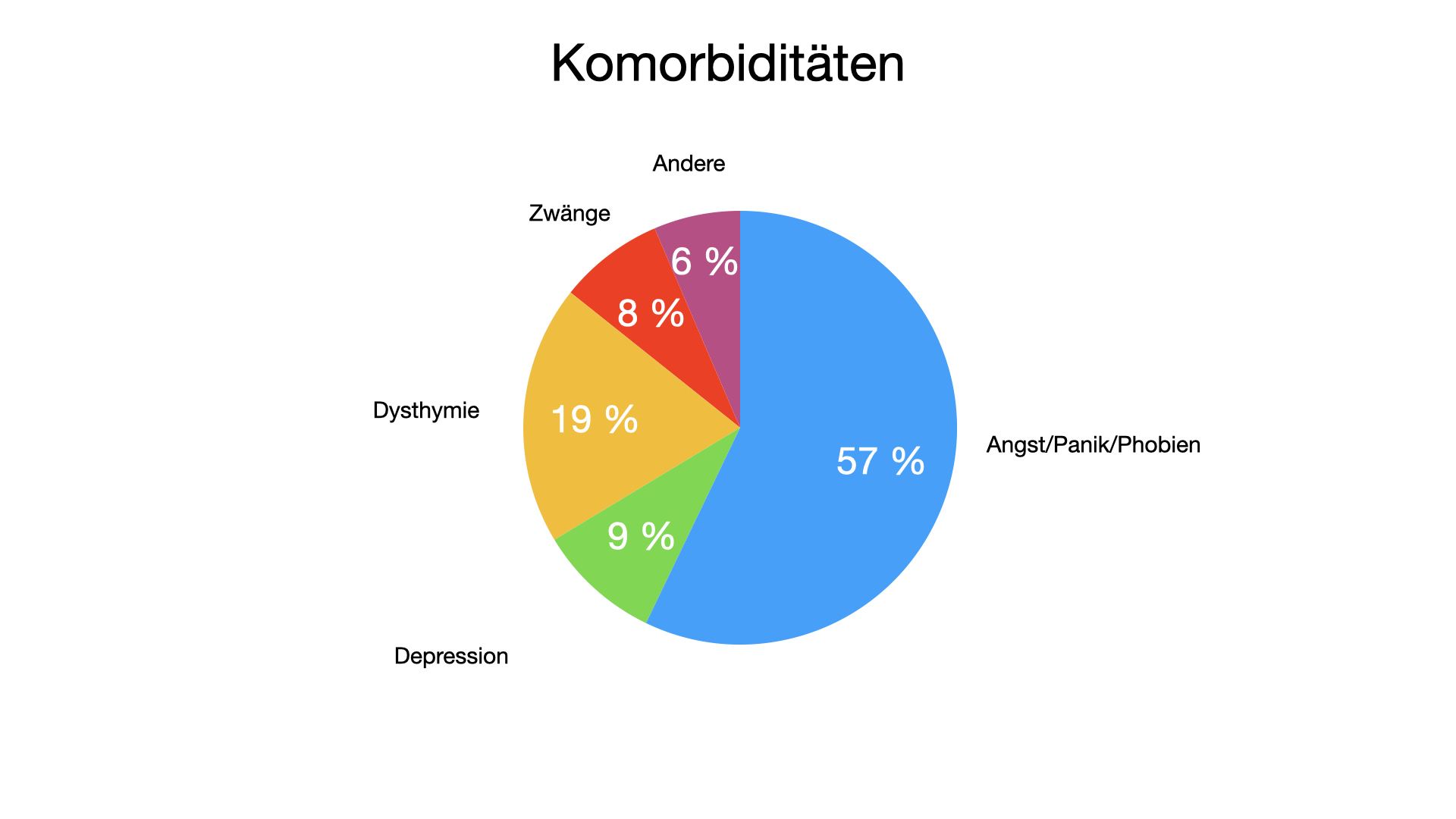
A distinction is sometimes made between primary and secondary forms.
- Primary: without other concomitant diseases
- Secondary: in the context of other physical and mental illnesses, e.g. depression, anxiety, psychoses, physical illnesses.
ICD 10
"A rare disorder in which a patient spontaneously complains that his or her mental activity, body, or surroundings have changed in quality, and are experienced as unreal, distant, or automated. Among many other phenomena and symptoms, patients most often complain of loss of emotions, alienation and detachment from their own thinking, from the body, or from the surrounding real world. Despite the dramatic form of these experiences, the patient in question is aware of the unreality of this change. The sensorium is normal, the possibilities of emotional expression intact. Depersonalization and derealization phenomena may occur in the context of schizophrenic, depressive, phobic, or obsessive-compulsive disorder. In such cases, the diagnosis of the foreground disorder should be made."ICD 10
DSM V
A. The presence of persistent or recurrent experiences of depersonalization, derealization, or both:
- Depersonalization: experiences of unreality, detachment, or experiencing oneself as an outside observer with respect to one's own thoughts, feelings, perceptions, body, or actions (e.g., perceptual changes, disturbed sense of time, unreal or absent self, emotional and/or physical stupor).
- Derealization: experiences of unreality or detachment with respect to the environment (e.g., persons or objects are experienced as unreal, as if in a dream, as if in a fog, lifeless, or visually distorted).
B. During depersonalization or derealization experiences, reality testing remains intact.
C. Symptoms cause clinically significant suffering or impairment in social, occupational, or other important areas of functioning.
D. The disturbance is not a consequence of the physiological effects of a substance (e.g., substance of abuse potential, medication) or a medical factor of illness (e.g., seizure).
E. The disturbance pattern is not better explained by another mental disorder such as schizophrenia, panic disorder, major depression, acute stress disorder, post-traumatic stress disorder, or another dissociative disorder.
Diagnosis
Diagnosis
The diagnosis can be made by an experienced physician, especially psychiatrist/psychotherapist. Questionnaires and structured interviews can be helpful.
A very simple distinction is proposed byBritish colleagues. It is based on only two questions:
"In the last two weeks, how often have you been disturbed by the experience of being
- Your surroundings feel detached or unreal, as if there is a veil between you and the outside world
- you feel out of the blue, as if you are not real, or as if you are cut off from the world."
These questions are answered in three strengths
- not at all =0
- some days =1
- more than half of the days =2
- almost every day =3
Now you only have to add up. A maximum of 6 points is possible. Three points or higher indicate probable depersonalization/derealization.
Other tests are e.g.
- Cambridge Depersonalization Scale
- Dissociative Experiences Scale (DES)
- Depersonalization Severity Scale
Cambridge Depersonalization Scale
One of the most commonly used questionnaires for derealization and depersonalization is the Cambridge Depersonalization Scale.
You can find the German version as an online questionnaire here. It takes about 10 minutes to fill out. You will receive the result immediately at the end.
Important: Questionnaires have only a supporting diagnostic function. As shown, the conversation with a competent colleague is crucial.
Differential diagnosis and concomitant diseases
Exclusion examinations
A number of physical diseases should be ruled out:
- Inflammatory brain diseases
- Rheumatic diseases
- Thyroid disorders
- Brain injuries
- Epilepsies
- Severe sleep disorders
Online investigation
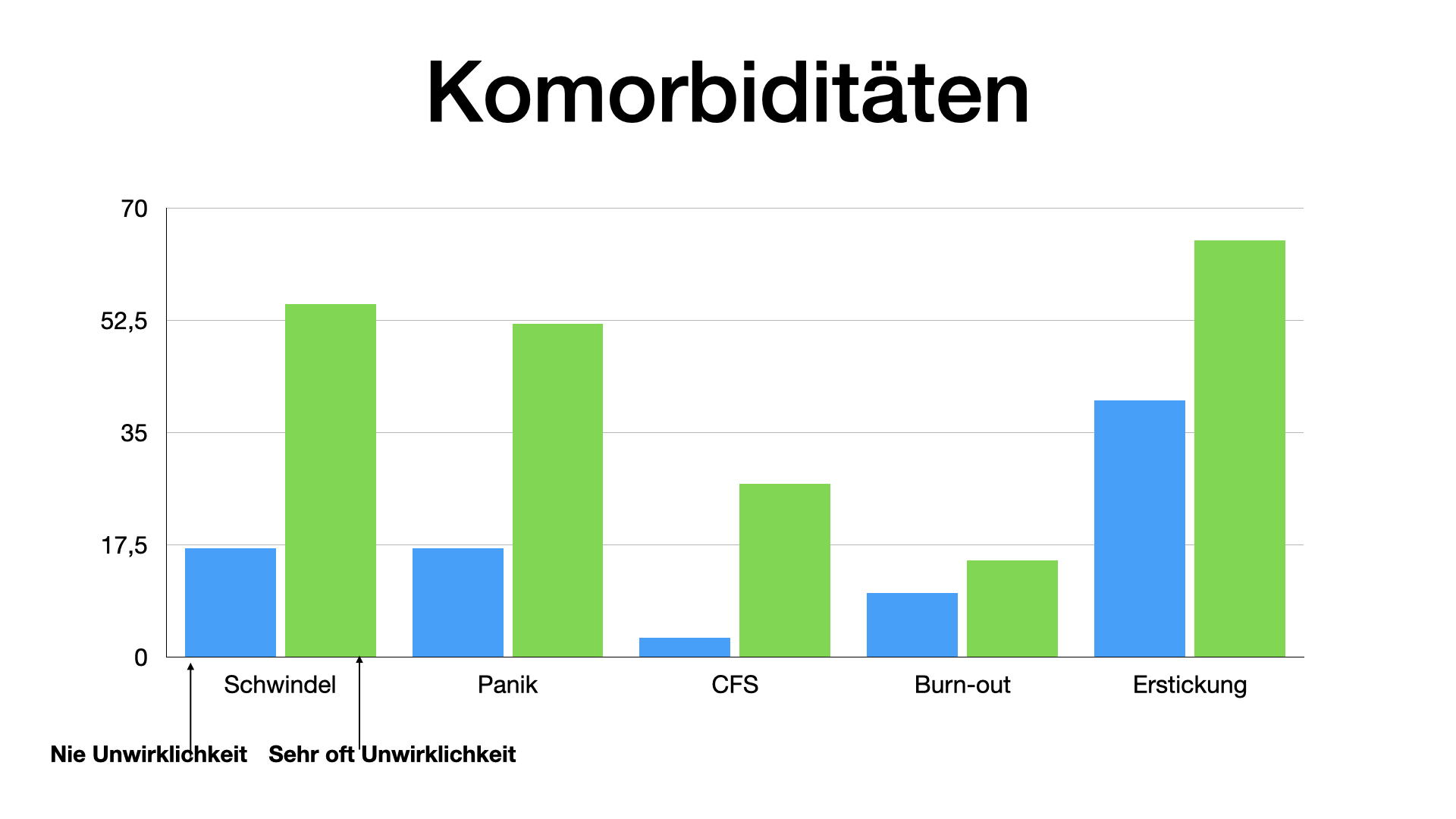
In a separate online survey with approx. 4000 participants, the questions asked included "absorbent cotton feelings" or "whether everything was unreal". Whether these participants actually suffer from derealization or depersonalization cannot be determined with certainty on the basis of answering a single question. Nevertheless, there is a certain probability that this is the case, since the other complaints also correspond well with the complaints that patients with derealization and depersonalization generally complain of.
Of the online group, 1314 answered "never" and 288 answered "very often" regarding "absorbent cotton feelings or "whether everything is unreal."
The following complaints occurred more frequently in the "very often" group:
- Dizziness
- Panic
- exhaustion, CFS, burnout
- history of suffocation
- Drowsiness
- Anxiety
- Palpitations
- Breathing disorders
- Cold hands
- and other functional symptoms
Triggers
Panic, drugs, trauma
Sustaining factors
Sustaining factors
Many unfavorable life circumstances (e.g., tension, insecurity, unresolved conflicts) can promote chronification. However, one factor should be emphasized. As is often the case with functional disorders, internal catastrophizing tends to perpetuate the complaints.
Finally, excessive attention to the phenomenon is very unfavorable. The more the inner focus is on the strange feeling, the stronger it becomes.
Conversely, any form of relaxation and inner distance is favorable.