Fibromyalgia means pain all over the body, fatigue, sleep disturbances, gastrointestinal complaints, swelling and many puzzling functional complaints. But as severe as the symptoms are, no physical findings can be found.
What is this disease? How can it be diagnosed with certainty? Above all, how can it be treated successfully? These are the questions we are dealing with here.
You will find comprehensive information here. Our knowledge comes mainly from our daily work with several thousand patients we have treated in over 20 years. The most important thing first: Fibromyalgia is treatable!
To get a quick overview, you can, for example, take our video learning course. Also a look at one of the introductory films or one of the video examples helps to get oriented. If you want to go deeper, you can also read one of thebooks.
A small self-test can help orient you if you are not sure if you suffer from FMS.
How we treat specifically, you will find under special therapy. What you may only read between the lines: We enjoy treating patients with this clinical picture and are happy with you about their successes!
Introduction
Introductory film
Introductory lecture
Diagnosis
Long time until diagnosis
Until recently, it took an average of 5-7 years for fibromyalgia syndrome to be correctly diagnosed. Fortunately, this time span has become shorter in recent years.
Nevertheless, every year that passes is too long, as the disease continues to chronify, meaning the symptoms continue to spread, not only causing unnecessary suffering, but also becoming more difficult to treat.
Therefore, it is of tremendous importance to know how to diagnose this disease with confidence.
The American College of Rheumatology, in1990, made proposals for this purpose, which for a long time was the only criterion for diagnosis. In 2010, new proposals were developed, which above all relativized the importance of the tender points.
At the same time, an S3 guideline is available for Germany, which was developed in 2008, updated in 2011 and 2017.
Orientation short test
Here is an orienting self-test that can give an indication of whether fibromyalgia syndrome is likely in your case.
Of course, such an initial test in no way replaces a thorough diagnosis by an experienced physician!
Tender Points - often misunderstood pressure points
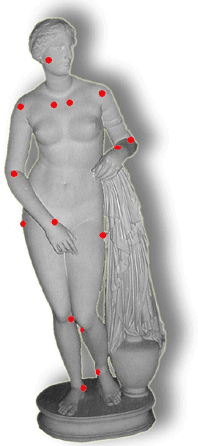
Equally significant for the understanding and diagnosis of this disease are the pressure points, the "tender points".
You can best understand the phenomenon by doing a little experiment. Feel the spot where the muscles of the forearm join the tendons at the elbow and press hard with your thumb. You may have to search a bit until you find these spots on the front and back of the elbow.
If this pressure hurts, you have found a "tender point". However, you do not have to get a fright now: One tender point does not make fibromyalgia! The two points on the elbow are sensitive to pain in most people. They are approximately the places, which hurt also with the "tennis elbow" so pulling. In the case of tennis elbow, however, the damage is located just next to it in the transition from the tendon to the bone.
If it hurts on the other side, one speaks gladly of the golfer's arm. By the way: Most people who suffer from the complaints play neither golf nor tennis!
Now, of course, there are not only these two muscle-tendon transitions. In principle, any muscle can be affected. Before you read on, you should estimate how many muscles you have? It is exactly 424 in words: four hundred and twenty-four! In addition to these striated muscles, which we can control consciously, there are countless other longitudinally striated muscles that work in the digestive tract, for example.
About 40% of the body weight consists of muscles. This makes them the largest organ of the human body. Fortunately, the pain points do not occur in each of these muscles. There is no agreement on the exact number that are usually affected. Up to 75 pain points have been described, but they are not all equally important.
If you look closely at the figure, you will notice that not only the transitions from muscle to tendon are drawn. Another transition on the rib cage, namely the cartilage-bone junction in the area of the ribs can cause pain. If you palpate it from the outside, you can feel it under the skin or below the pectoral muscles. Often, each cartilage-rib junction is affected.
Since the ribs are not the same length, but get shorter and shorter from top to bottom, the pain points are located further and further out, as seen from top to bottom. This makes them easy to distinguish from other sensitive points.
These tender points in the chest area are significant because they are probably responsible for the very unpleasant chest pain that many fibromyalgia patients suffer from. Often enough, they are so severe that the discomfort is mistaken for a heart attack, and the afflicted people are admitted to an intensive care unit.
Still a second area is an exception to the rule: in the area of the small wrists and ankles, the surrounding tissue may be affected. This is a condition that is accompanied by a painful restriction of movement.
I assume that in the meantime you have checked yourself whether the indicated areas hurt. Presumably, during this check, you found that many of these tender points cause discomfort if you just press hard enough. Muscle-tendon junctions are by nature more sensitive than the center of the muscle, so-called "trigger points", which have nothing to do with the pressure points of fibromyalgia. These are palpable hardenings in the muscles.
There has been much discussion in the past about the significance of tender points. Currently, my understanding is this: Fibromyalgia syndrome is characterized by an abnormal lowering of the threshold for stimulation. One becomes overly sensitive to pain. This is only particularly pronounced in the area of the tender points.
But: It ultimately affects the entire body. Every bump hurts practically everywhere!
Problem

With fibromyalgia syndrome, there are countless painful parts of the body. Sometimes it hurts literally "everywhere". Among the abundance of conceivable points, one has agreed on 18. Of these, in turn, 11 should be particularly sensitive to make the diagnosis.
Research showed that the ACR criteria have an accuracy of almost 90%. The degree to which the tender points are painful is highly consistent with physical and psychological discomfort. If the tender points are very sensitive, the overall threshold of irritation is usually also significantly lowered.
But there is also a problem. The examination of the pressure points (tender points) is anything but objective. It is not so easy to press exactly with four kilograms on one of these points and, moreover, displacements of only a few millimeters already make a decisive difference.
Even the use of pressure measuring devices (dolorimeters) does not solve this problem. In addition, patients suffering from pain of a different nature also have positive tender points in the same way.
Attempts were made to solve the problem by introducing so-called control points, which, unlike tender points, must not be sensitive to pain. But these points, e.g. on the forehead, are just as hypersensitive in two thirds of fibromyalgia patients.
Finally, there are patients (often men) who have the full symptomatic picture, but only 9 or 10 tender points are positive. Shouldn't this be called FMS? But what do these patients have then?
In short: Many scientists today see the Tenderpoints with critical eyes. They assume that the Tenderpoints were taken too important in the early years. In contrast, considerably more attention should be paid to the other symptoms (exhaustion, psychological restriction, concentration disorders, gastrointestinal problems, etc.).
Therefore, tender points were no longer included in the "hard criteria" for fibromyalgia syndrome. We regularly examine these pressure points, however, we only evaluate them as an additional and complementary symptom that rounds off an overall picture.
Current clinical criteria for diagnosis
Central are the spread pains. These can now be determined with the help of a regional pain index (see graph). Widespread pain is considered to be present in 7 or more of the 19 regions.
Symptom severity score
The symptom severity score assesses how severe the symptoms are. A maximum of 12 points is possible. 5 or more should be positive. The term "physical complaints" refers primarily to the multitude of functional complaints.
| Exhaustion | 0 | 1 | 2 | 3 |
| Non-restful sleep | 0 | 1 | 2 | 3 |
| Mental impairment | 0 | 1 | 2 | 3 |
| Physical complaints | 0 | 1 | 2 | 3 |
(0 = no complaints, 1 = mild, variable complaints, 2 = moderate, frequent complaints, 3 = severe, debilitating complaints)
No other reasonable explanation
And of course, no other disease should be present, which would explain the overall symptomatology. - This means that sufficient research has been done!
Differential diagnosis - What else can it be?
Not all extended pain is fibromyalgia!
Possibly you will have discovered a whole series of the symptoms described so far. But this does not automatically mean that you also suffer from fibromyalgia. Several diseases, which can easily be confused, cause similar symptoms. Therefore first some rules of thumb for orientation. If you have one or more of the following symptoms, you most likely do not have primary fibromyalgia. In any case, you should seek further evaluation to arrive at a correct diagnosis. In principle, one should not self-diagnose. However, as a sufferer, you can clarify whether there is a reasonable suspicion, which you can then have clarified by a specialist.
No sign of fibromyalgia!
- Clear changes in X-rays, computer tomogram, during ultrasound examination, etc.
- Long-lasting fever (over 38°C), pronounced muscle weakness, paralysis, visible redness, overheating around the joints or pain in (!) the joints, changes in the shape of muscles or joints.
Risk of confusion
I would like to mention some diseases that can easily be confused with fibromyalgia. A number of them are characterized mainly by concomitant inflammation or typical laboratory changes.
- Polymyalgia rheumatica
- Muscle inflammation
- Rheumatoid arthritis (inflammatory rheumatism of the joints), especially an incipient rheumatoid arthritis is often without laboratory changes and can often be difficult to distinguish from a fibromyalgia syndrome.
- Connective tissue diseases (med. collagenosis): Sjögren's syndrome, lupus erythematosus, polymyositis, dermatomyositis and others.
- Hormonal diseases: Hyperthyroidism and hypothyroidism or hyperparathyroidism.
- Infections, e.g. Epstein-Barr virus, hepatitis virus or Borrelia bacteria
The right contact person to rule out these diseases is, for example, a rheumatologist, endocrinologist and, of course, the family doctor.
Side effect medication
Acute damage to the musculature can be caused by a whole range of medications, which are accompanied by massive pain. If you take such a medication, please do not fear now that you will inevitably get (secondary) fibromyalgia. Fortunately, this happens only invery rare cases. However, it is different if you already suffer from the typical symptoms of fibromyalgia and at the same time take one of the mentioned medications. In that case, you should talk to your doctor about trying to stop taking the medication. After a few weeks, the complaints should then improve.
The following preparations may be associated with diffuse pain:
- Cholesterol-lowering drugs (fibrates, lovastatin).
- Narcotics,
- Diuretics (bumetamide, metolazone)- Asthma medications (salbutamol)
- Gout medicine (allopurinol)
- Emetics (emetine)
- Hemostatic agents (epsilon-aminocaproic acid)
- Antirheumatic agents (D-penicillamine)
- Antimalarials (chloroquine)
- Antiestrogens (treatment after breast cancer)
- a.o.
Inflammatory rheumatism
Fibromyalgia not infrequently occurs after an inflammatory rheumatic disease. This can be a classic rheumatoid arthritis ("joint rheumatism") or other rheumatic diseases. According to a study, a part of rheumatic patients suffer from fibromyalgia at the same time: 6.6% in rheumatoid arthritis, 13.4% from systematic lupus e., 12.6% in ankylosing spondylitis, 10.1% in osteoarthritis, 12% in Sjögren's syndrome and 25% in vaculitis.
In recent years, we have frequently seen patients with polymyalgia rheumatica who developed fibromyalgia syndrome following severe inflammatory rheumatism.
Fibromyalgia after polymyalgia
Fibromyalgia as a concomitant disease
Sometimes patients with severe inflammatory diseases also suffer from fibromyalgia symptoms. This is not only the case with classic joint rheumatism (rheumatoid arthritis), but also with other rheumatic diseases (e.g. lupus erythemotodes). The chronic pain and the countless stresses caused by the disease are likely to be the decisive triggering factors.
Of course, there are more diseases in which fibromyalgia syndrome often occurs simultaneously. Examples would be migraine, depression or anxiety disorders. In all these cases, two or more diseases are present at the same time.
In former times one spoke in this connection gladly of a "secondary" Fibromyalgie, since another illness released the FMS. This distinction is no longer made today, since ultimately something (back pain, sleep disorders, injuries, etc.) always triggers the complaints.
Fibromyalgia and CFS
Chronic Fatigue Syndrome (CFS) is characterized by debilitating mental and physical exhaustion/exhaustibility and other symptoms that vary from individual to individual.
The exhaustion must last for at least 6 months and lead to a severe reduction in performance compared to what was previously usual. Contrary to what the name suggests, exhaustion is only a part of CFS.
The clinical picture includes headaches, sore throat, muscle and joint pain, concentration and memory disorders, non-restorative sleep, sensitivity of the lymph nodes, nerve twitching and tingling in the body, depression, ringing in the ears, visual disturbances, allergies, subfebrile temperatures, as well as a persistent worsening of the condition after exertion and much more.
In the majority of sufferers, the disease develops abruptly after a nameable event. Others report a gradual deterioration of their general condition. The symptoms may persist for years. Causes and disease mechanisms of CFS are not yet known. Immune dysfunctions, viruses, hormonal disorders, fungi, psychological factors, persistent stress or environmental toxins are discussed internationally as triggers.
It is asked again and again to what extent CFS and fibromyalgia actually represent separate clinical pictures or only different "varieties" of a superordinate disorder. Above all, the many vegetative disturbances that occur in both diseases indicate that a fundamental dysfunction in the control of the body at the hormonal and neuro-vegetative level is significant in both diseases.
Unlike CFS, however, immunological disturbances are less significant in fibromyalgia. Here, too, viral infections are repeatedly named as one of the triggers and a "banal" infection can significantly worsen the symptoms. This aspect plays however by far not the role as with the CFS.
A depressive basic mood is found in both diseases. While some colleagues put this fact in the foreground as the "secret" cause, this does not seem to us to be so correct. From our point of view, this factor is rather the consequence than the cause of the disease. In fact, one must assume an extremely complex relationship between physical and psychological factors.
All in all, the discussion about the "ultimate" cause will not be over for a long time. This is especially true if one includes the other diseases in the environment (MCS, irritable bowel syndrome, etc.). Recently, the proximity of CFSwith a number of respiratory disorders as well aspostural tachycardiahas come to our attention and seems particularly important.
"Larvalized" depression?

Since fibromyalgia is usually accompanied by pronounced mood swings, the question arises again and again whether the disease is perhaps a special type of depression, a so-called "larvierte" (disguised) depression. In this form of depression, the focus is not on the mood, but on a variety of physical complaints: Headaches, abdominal pain, dry mouth, heart trouble, and many other of the symptoms you have already encountered as accompanying complaints in fibromyalgia. It is, so to speak, "depression without depression."
From our point of view, it is exceedingly doubtful whether it is useful to mention these terms. Many researchers and clinicians reject the term "larval depression." However, we mention it here because it often comes up in connection with fibromyalgia syndrome.
However, whether or not one uses the term, there is certainly overlap between depression and fibromyalgia syndrome.
However, there are characteristic differences: the physical complaints in depression are usually more variable, diffuse and difficult to delimit than is the case with fibromyalgia. However, one thing is clear: In depression, the painful "tender points" are usually absent.
Physical symptoms
Pain, overstimulation, exhaustion

Once the disease has fully developed, those affected usually suffer from the following complaints:
- Constant pain and pain at rest are in the foreground. About half of the patients complain that they have pain everywhere. In addition to the spine, arms and legs are almost always affected. However, there are also cases in which only individual muscle areas (e.g., the shoulders) hurt in addition to the spine.
- Particularly sensitive to pain are certain muscle-tendon junctions, the "tender points" already mentioned. They have a prominent role in diagnostics (see there).
- A general irritability of the nerves is another symptom of the disease: hypersensitivity of the skin, smell, ears, etc.
- In addition to pain, the majority feel depressed, depressed or anxious.
- More than half of the patients suffer from pronounced tension headaches. Often these move from the back of the neck to the front of the head. A second "favorite" location is the eye/sleep area.
- Some patients have to endure a migraine in addition to the headache. Main symptoms are unilateral headache associated with nausea, light and noise aversion.
- In the morning, patients complain of marked stiffness of the joints and the feeling that they are swollen, although swelling is not always visible. Swelling also usually occurs around the eyes, cheeks, and fingers, and the nose is often swollen in the morning. Women suffer from feelings of tightness in the chest and abdomen. Before and during menstruation, these complaints can increase significantly and can progress to cramps.
- Exhaustion, lassitude and fatigue are the main symptoms of fibromyalgia. This massive fatigue is rarely absent and torments the patients very much. It is often so pronounced that regular professional activity is not (or no longer) possible.
- An occupation is made more difficult also by the often to be observed disturbance of the concentration: Drowsiness, memory gaps, a disturbance of the short term memory, the feeling of the "matt screen" or a general slowing down are complained of Fibromyalgie patients. Some sufferers have the impression that they are constantly beside themselves. In the American-speaking world, this "foggy state" is usually referred to as "fibrofog" (fog=fog).
- Sleep disturbances are just as common. Those affected have a light sleep, wake up often, cannot fall back asleep and, above all, do not feel refreshed from sleep.-burping, bloating, heartburn, increased bowel sounds, flatulence, diarrhea or constipation are rarely absent.
- Allergies are found in a surprising number of patients. These range from hay fever to asthma to severe cases in which there is an allergic reaction to virtually everything.
- Fibromyalgia patients are usually very sensitive to cold and report signs of impaired circulation: cold hands, feet or Raynaud's syndrome.
- Carpal tunnel syndrome is also common. This is a constriction of a nerve in the wrist area. As a consequence, severe pain occurs in the entire arm at night. 50% of all fibromyalgia patients suffer from carpal tunnel syndrome. 50% of patients with carpal tunnel syndrome suffer from fibromyalgia!
- Circulatory disturbances with violent dizziness are not dangerous, but affect the lives of many patients quite massively.
- Confusing for doctors and patients alike are the many so-called "vegetative" complaints that are typically associated with fibromyalgia. They can be understood as disturbances in the regulation of bodily functions.
Pain quality
Fibromyalgia patients often suffer from pain that they find puzzling because it is wandering, shooting in, burning, and delayed. The whole body can become hypersensitive. There seems to be no cure for this pain, and painkillers work no better than cough drops.
To understand how this happens, it is helpful to make a distinction that is commonplace in pain management, but curiously little known outside that field.
One must distinguish different types or "qualities" of pain:
Nociceptive pain
Nociceptors are understood to be pain sensors. They are often free nerve endings that are able to perceive damaging influences. Nociceptive pain is the classic or "normal" pain. It can be caused by joint wear and tear, i.e. osteoarthritis, fractures, injuries or, for example, abdominal pain.
Neuropathic pain
Something completely different is neuropathic pain, which can best be translated as nerve pain.
In fibromyalgia, it is true that there is no classic neuropathic pain, as in phantom limb pain, diabetic pain syndrome, or the pain that occurs after shingles. But often neuropathic parts are clearly recognizable.
- The pain continues to occur despite the removal of the causative damage and source of pain.
- It persists for days or weeks after the injury.
- The pain is accompanied by insensations and radiation.
- The place of origin and the place of perception do not always coincide.
- Pain changes in character: burning, electric, stabbing, tearing, etc.
- In addition to continuous pain, there are attack-like shooting pains.
- Weak stimuli can trigger violent pain.
- Pain becomes more severe even though the stimulus remains the same.
- The pain lasts longer than the stimulus.
Practical consequences
The distinction has drastic significance for therapy. While classic nociceptive pain responds well to analgesics and rheumatic drugs, these are ineffective in neuropathic pain! This fact cannot be repeated often enough, as it is very often overlooked. So neuropathic pain needs a different therapy.
So, in fibromyalgia syndrome, one must differentiate. If the neuropathic pain quality predominates, then one can mostly dispense with an attempt with aspirin, ibuprofen or diclofenac.
On the other hand, antidepressants, anticonvulsants (drugs against epilepsy) and morphines would be useful - mostly in low dosage.
In addition to diffuse pain (against which painkillers do not help), acute pain occurs from the cervical or lumbar spine, which may very well be treated with ibuprofen or diclofenac.
As always with such recommendations: Consult with your physician for specific steps.
| Medications | Nociceptive pain | Neuropathic pain |
|---|---|---|
| Pain rheumatoid medications | +++ | - |
| Opioids | +++ | ++ |
| Antidepressants | - | +++ |
| Anti-epileptic drugs | (+) | +++ |
| Cortisone | ++ | (+) |
| Neurolopetics | ++ | + |
Vegetative complaints
Fibromyalgia patients suffer from a variety of complaints that bring them into contact with almost all medical disciplines. Despite the intensity of the impairment, they are usually told that they have no or at most minimal findings. This discrepancy between complaints and findings then astonishes both doctor and patient. If this is initially perceived as puzzling, in the long run it is attributed to psychological processes. In short, the patient should seriously consider seeing a psychiatrist.
Patients usually feel unsettled by this. They themselves do not have the impression of being mentally ill. If they nevertheless take the advice and see the mental specialist, this therapy is rarely successful. Although they learn a lot about themselves and their life history, the complaints alone do not want to get better.
The reason for the confusion is not individual complaints, e.g. pain, but above all the multitude of so-called "vegetative complaints". They are so varied, unsystematic and "colorful" in their appearance that even well-meaning family doctors doubt the mental condition of their patients. A disease that causes so many different symptoms cannot exist...
Increased tendency to sweat, sensitive skin with excessive reaction to touch (dermographism), increased vein markings, circular hair loss, cardiac arrhythmia, breathing difficulties, unclear pain in the chest area with shortness of breath, susceptibility to infections, slightly increased temperature, numbness, "restless-legs", cramps in the leg muscles, trembling hands, irritable bladder, water retention, period pains, loss of sexual interest, impotence, hoarseness, difficulty swallowing, lumpiness in the throat, toothache, pain in the chewing muscles, hearing disorders, tinnitus, mood swings, irritability, etc.
What all these complaints have in common is that there is no organic change in you. Laboratory tests, X-rays, computer tomography, etc. show no tangible result. Does the absence of "objective" findings mean that the complaints must be attributed to the soul after all? I think that this is an oversimplification that does not do justice to the factual situation. The vegetative disorders have their own dynamics, which, however, are still insufficiently appreciated in medicine.
So what are the backgrounds of these many impairments, large and small? Let's first look at the basics, the autonomic nervous system.
More about functional disordersand the autonomic nervous system
Water retention, swelling, edema
Many women with diffuse pain in the body report strange swellings. They suffer from "thick eyes" in the morning, swollen fingers, heavy legs and the feeling that the skin is too tight. "As if I am locked in a diving suit," is how they feel in pronounced cases.
The background is a problem with the tissue water, the lymph. If congestion occurs here, these peculiar swellings appear.
In the beginning, only depressible dents can be seen. Later, however, fat is also deposited. The skin becomes thicker, orange peel skin and "cellulite" appear, and above all the weight goes up a little.
Likewise, pain is then added and an accumulation of bruises ("blue spots") at the slightest bumps.
Fibromyalgia of the "edema" type
Carpal tunnel & Co.
Nerve bottleneck syndromes are extremely common in fibromyalgia. The best known is the so-called carpal tunnel syndrome.
It is a pressure damage of a nerve in the periphery of the body. The symptoms are manifold. They begin with insensations, increase to numbness and pain, and end with paralysis.
The symptoms are favored by repeated uniform movements (typing, musicians).
Risk factors are: Alcoholism, diabetes, thyroid disease, pregnancy, female sex, middle age.
In fibromyalgia, especially diffuse edema is a major risk factor. Here I observe very close correlations. The more pronounced the edema, the greater the swelling in the channels through which the nerves "squeeze".
Although the symptoms are often quite clear (e.g., in the case of carpal tunnel, nocturnal pain in the whole arm), the diagnosis often takes quite a long time. Best diagnostic method: measurement of currents in the nerve - neurography and electromyography.
Standard therapy: immobilization, night splint, anti-inflammatory drugs, if necessary short-term cortisone, at the end surgical widening of the canal.
In fibromyalgia with concomitant edema, anti-edematous therapy is usually exceedingly successful. This is all the more important because the complaints, e.g. in carpal tunnel syndrome, also occur on both sides and can recur in the same hand even after surgery. See also: Lipedema
Blurred vision
Fibromyalgia patients often complain of a confusing visual disturbance. You see alternately well or poorly. Sometimes the vision is blurred and out of focus, then you see again without any impairment.
They often report that they have difficulty reading the newspaper right after getting up in the morning. In the course of the day, however, this quickly improves.
A visit to the ophthalmologist brings little clarity. Usually he can find nothing. "Everything without findings" is the diagnosis, or the complaints would have nothing to do with an existing myopia, for example.
During our own examination we could see a connection to the respiration. Similar complaints are also found inchronic hyperventilation.
Mental symptoms
Body or soul

Undoubtedly one of the most frequently asked questions about fibromyalgia is, "Is the disease mental?"
Leading researchers worldwide agree that fibromyalgia is not a disease caused by the soul. This fact is very important to me because most fibromyalgia patients are told at some point in their medical history that they are hypertensive, neurotic, or merely imagining their symptoms. For the affected patients, this is usually a severe blow. At best, they only feel misunderstood; at worst, they doubt their mental condition and feel guilty about the disease.
This view is certainly wrong! If you yourself should suffer from this disease, please do not let yourself be persuaded that everything is only due to your soul. Your disease is hard enough to bear, and you don't need to burden yourself with additional misconceptions.
Fibromyalgia is not a pure expression of the soul!
On the other hand, this does not mean that psychological factors do not play a role in the disease. Often people are found who are particularly sensitive and at the same time willing to perform. Insecurities in childhood or an insecurity of the parents are also very often found.
And there are consequences: A disease that interferes so deeply with everyday life naturally has an impact on the psyche. Like most chronic diseases, fibromyalgia often triggers depression, sadness or depression. As a result, the low mood again has a worsening effect on fibromyalgia.
We are therefore dealing with a complex control loop in which the mental state - in addition to many other factors - is involved, but not the sole cause of the disease!
In summary, we can say that mental and physical factors are closely intertwined in fibromyalgia. At times when you are unwell, when you have poor self-esteem, you will suffer more from the disease. Likewise, the physical symptoms also affect your mood. However, a positive mood helps you to bear the pain better
In each person, physical and emotional factors are different. But whatever this relationship is: You yourself are not "to blame" for your illness!
This fact is very important to me, because in the course of their "patient career" most fibromyalgia patients have reached the point where they begin to doubt themselves: "Am I crazy in the end?" Or, "Isn't it all my own fault?"
The cause of such despair, however, lies less in the disease itself than in the doctor-patient relationship.
With this, I would like to simultaneously emphasize and relativize the importance of psychotherapeutic treatment. Fibromyalgia is not a psychologically caused disease. Accordingly, it cannot be cured exclusively by psychotherapeutic methods. On the other hand, psychological factors usually play an important role in the development and course of fibromyalgia. This means that it is necessary to consider the emotional aspects of the disease as well.
Not every fibromyalgia patient needs psychotherapy for this reason - but for some, this therapy does a lot of good. Any significant change in behavior, an intense conversation with friends, or a nice vacation can be "psychotherapeutic." So it is about how you can take care of your own psychic needs in the context of the disease.
Sleep disorders
Sleep disturbances are one of the most unpleasant complaints of fibromyalgia. If you are affected, then you know it: You fall into bed dead tired and probably fall asleep quickly. But then: After a few hours, at the latest 2 or 3 o'clock in the morning, it is over with the slumber. You roll from one side to the other. Everything hurts! You can't sleep, and if you do doze off for a moment, a new pain or your bladder wakes you up.
In the morning you feel exhausted, as if you had been chopping wood all night or you had been drinking excessively.
From our point of view, sleep disturbance is ultimately based on an old protective mechanism: in earlier times, sleep involved risk. Not sleeping was certainly better than relaxed slumber in case of threat (e.g. large animals).
Fibromyalgia and partnership

Every illness means an influence on the partnership. If one can rather cover up an illness to distant persons, the partner gets to know the complaints very closely. Next to the own person, he or she is affected the most. This does not always have to be the spouse. Girlfriends or boyfriends, parents, children, siblings inevitably suffer as well. Men in particular often find it difficult to accept that their partner is not fully capable.
Even a 14-day cold can have an impact on a partnership. Months or years of illness are one of the heaviest burdens a relationship has to endure. It is almost as if the illness lives in the household as an unwanted and invisible person.
Often the ill person then suffers from feelings of guilt. But the partner also gets into a difficult emotional situation. He tries to support and help where he can. But his efforts come to nothing with fibromyalgia. This creates disappointment, anger and a hidden inner reproach. Since a fibromyalgia sufferer cannot do anything for the illness, the life partner himself gets feelings of guilt. So finally both are entangled in mutual reproaches and feelings of guilt. Under it the joy of life and the relationship quality suffers. Feelings grow cold and the illness is now compounded by an impairment of the partnership.
We have great respect for the responsible and considerate way many couples treat each other. The daily confrontation with the ailments requires great human maturity from both of them. It is not surprising if one occasionally despairs at the oversized task.
Fibromyalgia and sexuality
If you have a toothache, you don't write love letters. This fact is self-evident to most people. But a hole in the tooth can be seen and it can be fixed. With fibromyalgia it is different. The pain usually lasts for a long time and no defect is visible from the outside.
Usually women suffer from fibromyalgia and have to make their husbands understand that they do not feel like tenderness or sexuality under these circumstances.
Our experience is that both men and women suffer from two things in particular:
- They feel no sexual need whatsoever.
- Physical touch and sex are usually unpleasant or painful for them.
Despite these difficulties, affected couples do not have to give up satisfying sexuality. Both partners should know that the problem is primarily caused by the disease itself. As a rule, the sick partner has not lost interest in sex, but is merely affected in phases by the disease. If you should suffer from fibromyalgia yourself, try to make this clear to your partner.
- Talk about the subject. Sexuality must not be a "sacred cow"!
- There are good and bad times for sex. If you feel completely smashed in the evening, you are guaranteed not to feel like it. Other times (early morning, midday) are often much more pleasurable!
- Prepare for tenderness together, both internally and externally: A warm bath alone or as a couple, candles, nice music....
- Sexuality is by far more than just intercourse. Do not try to force an orgasm. If intercourse is uncomfortable or painful for you, agree with your partner to forgo it once and enjoy the closeness with him or her as well as other forms of tenderness instead.
- Like pleasurable eating, sexuality also thrives on variety. A different environment, different positions or variations of the already familiar create new excitement.
- Do not be inhibited to inform yourself. There is a lot of good literature on this subject.
Causes
Stimulus threshold reduction - Central sensitization

Increased sensitivity may be at the core of FMS symptomatology.
This can be illustrated by the pain threshold of the teeth. If you chew vigorously, a single tooth is subjected to a pressure of 50, perhaps even 100 kiloponds. The temporomandibular joint is then subjected to almost a ton of stress. Despite the enormous forces, this is not painful. But it is different when a cavity has sensitized the tooth. If one avoids going to the dentist, high sensitivity often develops within a few days. The pain threshold can drop so low that even the coolest breath of air when inhaled causes unbearable pain. This is to illustrate that the range of sensitivity levels is exceptionally wide. Robust insensitivity and high-grade sensitivity are part of our being.
The following study is interesting in this context: patients with FMS were compared with a control group of healthy subjects using functional magnetic resonance imaging (fMRI). Thereby it is possible to measure the cerebral blood flow in different pain centers. Both groups were irritated with a small pain stimulus and the effect on the brain was checked. The first, unsurprising result was an increased irritability of the patients with FMS. Now the experiment was repeated, increasing the stimulus until the participants reported that the pain now corresponded to "7" on a 10-point pain scale. What was to be expected occurred. The FMS group already experienced the strength "7" with significantly lower stimuli. But the exciting thing was something else. Comparing the blood flow patterns of both groups at "7", there was no relevant difference here.
In other words, the quality of pain does not differ between healthy individuals and FMS patients. It is only felt much earlier!
Pain and fear
In the course of an FMS disease, many patients observe increased sensitivity in other sensory qualities as well. Usually this begins with increased sensitivity to noise and light. A spouse seems to close doors louder, it becomes more uncomfortable when several people are talking at the same time, and it becomes especially difficult when trying to talk at a party while loud music is playing at the same time.
Increased sensitivity to touch and pressure is also very common. "Don't touch me so hard, please," is a saying that many spouses know well enough. In a small group of severely affected individuals, this can go much further. Even a gentle squeeze of the partner with the hands, can already lead to a violent wince. A reaction that often leads to incomprehension. ("What do you have now again?").
Childhood imprints - Lack of security

Practically all physicians, psychotherapists and psychologists who deal with FMS can confirm this experience: Very often, those affected describe difficult circumstances in childhood. One hears particularly often about beatings, violence, neglect or even sexual abuse.
Children can only defend themselves to a limited extent against such terrible living conditions to which they are helplessly exposed. But they can try to adjust to them. One form of response is to develop a heightened sensitivity in order to recognize the threat at an early stage. However, this heightened sensitivity is one of the risk factors for developing FMS.
However, another experience can also lead to the heightened sensitivity: Children experience parents as overprotective, worried, and insecure. They are in constant worry that something might happen to a child. Such experiences can also irritate children: They don't know why parents are like this and interpret behavior that way: The world is dangerous!
Depression and anxiety
Hardly any fact is as well studied as the connection between depression and FMS. Depending on the study, the information about the percentage varies. Between 30 and 80% of fibromyalgia patients suffer from a depressive illness at the same time. Depression also has an unfavorable effect on the course of FMS. It is possible that the same genetic disposition ("hyper-sensitivity") is a risk factor for both fibromyalgia and depression and anxiety. The question of whether the depression and pain came first or vice versa is akin to the chicken and the egg question. The two unfortunately reinforce each other.
But the research also shows something else: there is a large group of patients (between 20% to 70%) who have never been depressed. Their mood impairment is usually due to the pain.
Stress hormones
There are numerous hormones that may play a role in FMS. For example, changes have been described in growth hormone, adrenaline, and especially in the regulation of cortisone. As always in science, the results are not consistent and some are contradictory. But it seems quite likely that with regard to cortisone there is a two-stage process. In a first phase, chronic stress (pain, physical or psychological strain) initially causes increased production of cortisone. In a second phase, this regulation is exhausted with decreased cortisone levels and a reduced response of cortisone regulation to stress.
These considerations are significant because cortisone is one of the hormones that sets the body up for increased performance. It is produced during periods of stress (fight or flight) and instantly makes us more physically and emotionally resilient. In an interesting experiment, women were given either cortisone or an ineffective placebo before a stressful test task. The cortisone group felt significantly less stress afterwards than those who had only received a placebo.
If one considers the symptoms of a cortisone deficiency (tiredness, fatigue, dizziness, abdominal discomfort, etc.), a connection with the regulation of cortisone seems quite likely. But beware of quick fixes! Taking cortisone tablets, which leads to quick results with rheumatism, is unfortunately not helpful with FMS.
Again, an exception: sometimes FMS occurs together with an inflammatory disease, e.g. rheumatism. In such cases, taking cortisone naturally improves the symptoms, but this has nothing to do with FMS.
Thyroxine & Hashimoto's
In fact, it is also my clinical experience that there is often a correlation between thyroid gland dysfunction and pain. Both hypothyroidism and hyperthyroidism, as well as auto-immune thyroid disease (Hashimoto's thyroiditis), appear to be risk factors for FMS. However, this has not yet been scientifically proven. Appropriate studies with a sufficient number of participants are still missing. Taking thyroid hormones does not usually affect pain. Of course, one should pay attention to a correct adjustment of hypo- or hyperthyroidism.
Sympathetic nervous system - Parasympathetic nervous system
Simplified, our body has two different nervous systems. On the one hand, there are the nerves that you need at the moment to hold this book in your hands or to transmit the command to turn the page. These are assigned to the "somatic" nervous system (soma = body). This includes all the nerves that convey information to us from our sense organs about the external world (sight, hearing, smell, taste) and the internal world (pressure, touch, pain, internal organs).
On the other hand, there is the "vegetative" nervous system (vegetare = to grow, to animate), which is responsible for the processes that our will cannot directly control. These are the life-sustaining processes of the body such as metabolism, blood pressure, digestion, kidney activity, breathing, heartbeat, cell division, etc. When you make the decision to get up from a chair, you give a conscious command with the help of the somatic nervous system: "Get up with the right foot first and three steps forward!". The autonomic nervous system then works in the background: increasing pulse and blood pressure, redistributing blood flow to the legs, restricting digestive activity, increasing muscle tension in the abdomen, etc.
Within the vegetative nervous system there are further subdivisions. This is once the nervous system of the digestive organs ("enteric nervous system"), which provides for the regulated course of food utilization. It is often referred to as the "autonomic" nervous system, since we can influence it little or not at all. In addition, a distinction is made between the sympathetic nervous system, which makes us active, able to perform and ready to fight, while the parasympathetic nervous system conversely supports rest, relaxation and regeneration.
In fibromyalgia syndrome, there are numerous symptoms that can only be explained by a disturbance of the autonomic regulation. On the one hand there are the manifold gastrointestinal complaints, disturbances of blood pressure regulation, temperature regulation, regulation of sweating, bladder control, muscle tension and many more. These vegetative disturbances are very debilitating. Many sufferers have the impression that their body no longer obeys them. Every day new confusing complaints appear. It is typical that these regulatory complaints are difficult to measure. Blood pressure fluctuations are easy to determine, but disturbances in breathing, digestive activity, bladder activity or circulation are difficult to objectify. Laboratory tests, X-rays, computer tomograms or ultrasound always show only normal values. Nevertheless, these changes are real and - as already mentioned - not imaginary.
Different types of dysregulation are currently emerging: Affected persons with an overshooting sympathetic activation and those with a clearly reduced one. The first group shows a rapid stress reaction with blood pressure and pulse increase, an immediate and exaggerated general activation, while in the other group this is exactly the opposite. Obviously, there is a disturbance of the complex regulation that every conceivable external challenge poses to us. The differentiated, balanced control of muscle tension, pulse, blood pressure, respiration up to increased attention and mental tension is out of balance in FMS.
It is obvious that there are not only two types of FMS. Probably the number of subgroups is much higher; however, we are only at the beginning of research here.
Therapy
Disappointing painkillers

While hopes were initially placed predominantly on pharmacological (drug) therapy, it is now clear that these have largely disappointed as a sole measure. Drugs therefore play only a minor role in our therapy model.
Patients do not respond to either peripheral or central analgesics with definite pain reduction. Even the WHO step-by-step regimen (see adjacent) fails in fibromyalgia patients. Sufferers complain mainly about the side effects, without achieving a sufficient main effect. Antirheumatic drugs - anti-rheumatic drugs - also usually fail to achieve the desired effect.
Painkillers disappoint, among other things, because fibromyalgia syndrome is primarily a disorder of pain processing. An increased influx from peripheral nociceptors is not given or only to a small extent.
Clarity in mind, myths dispelled
Fibromyalgia is a clear-cut disease, and you are not to blame for the fact that the disease is still little known. Although sufferers are mentally unwell, this does not mean that you are "crazy".
Fibromyalgia is a disease that severely affects life, but on the whole does not cause any change in the structure of the body. There are never late damages, changes in the joints, crippling, etc. You will certainly never be in a wheelchair because of this disease.
The diagnosis of fibromyalgia syndrome is relatively simple. Therefore, once the correct diagnosis has been made, refrain from further extensive examinations. However, an acute inflammatory disease should be excluded. For this purpose, a few relatively simple laboratory tests, as performed by any general practitioner, are sufficient (e.g., blood count, erythrocyte sedimentation rate, rheumatoid factor, CRP, protein electrophoresis, immunoglobulins). Learn to accept that there are no tangible physical changes behind the disease. The more you get tested, the more random results there are. So there tends to be more ambiguity and confusion. Or, to take up a comparison again: If the traffic breaks down, you can examine the individual cars no matter how closely. That's not the reason!
Nothing works with violence!
Fibromyalgia is a clear-cut disease, and you are not to blame for the fact that the disease is still little known. Although sufferers are mentally unwell, this does not mean that you are "crazy".
Fibromyalgia is a disease that severely affects life, but on the whole does not cause any change in the structure of the body. There are never late damages, changes in the joints, crippling, etc. You will certainly never be in a wheelchair because of this disease.
The diagnosis of fibromyalgia syndrome is relatively simple. Therefore, once the correct diagnosis has been made, refrain from further extensive examinations. However, an acute inflammatory disease should be excluded. For this purpose, a few relatively simple laboratory tests, as performed by any general practitioner, are sufficient (e.g., blood count, erythrocyte sedimentation rate, rheumatoid factor, CRP, protein electrophoresis, immunoglobulins). Learn to accept that there are no tangible physical changes behind the disease. The more you get tested, the more random results there are. So there tends to be more ambiguity and confusion. Or, to take up a comparison again: If the traffic breaks down, you can examine the individual cars no matter how closely. That's not the reason!
Relaxation
Fibromyalgia therapy is about influencing regulatory circuits. An important starting point is breaking the cycle of pain, tension, anxiety and new pain.
This starts with an inner step: try to accept that the disease is currently stronger than you and cannot be fought by force. Perhaps you are confused now, since I just advised you to actively fight the disease. This is indeed correct, but it is not possible to do so in a combative manner. The disease still belongs to you and forms a part of your personality, just as there are character traits that you value less in yourself. You can be angry about this, but you cannot erase this part. On the contrary, the more you fight, the greater your inner tension will become and with it your complaints.
It only works in a friendly way: Team up with your body and look for a way out of the messy situation.
The same goes for external help. You will not find an expert who can rid you of all discomfort in one fell swoop. If you go to doctors with this hope, you will regularly be bitterly disappointed. In the attempt to attack the disease with harder and harder means, in the end everyone will be disappointed and everyone will be a loser. Such aggressive escalations happen frequently: Fibromyalgia patients are three times more likely to undergo surgery than comparable patients with other pain conditions. Some operations are unfortunately pointless and stem from helplessness and ignorance about the disease.
Therefore, form a team with doctors, physiotherapists, masseurs, etc. and look for a feasible way together. Everyone supports the other and no one is omniscient.
To make it easier, we have a guided, light relaxation instruction (meditative relaxation) in the online self-helparea.
Nutrition

Most fibromyalgia patients suffer from complaints in the gastrointestinal tract: belching, bloating, heartburn, bowel sounds, flatulence, diarrhea or constipation. "Irritable bowel syndrome" or "irritable stomach" is then the diagnosis.
Whether this is the cause or the consequence of the disease is a moot point and is ultimately irrelevant. What is important, however, is to treat these complaints successfully.
From our point of view, the most important thing is a proper diet. However, we do not want to offer you a new "miracle diet" or "fibromyalgia diet". It is about nourishing the digestive tract with a diet that is digestible for it. For us humans, this means using foods to which we have been able to adapt optimally in the course of evolutionary history.
This does not mean hamburgers, Sachertorte or cola drinks, but all foods that occur unchanged in nature: A raw, coarse, predominantly vegetarian diet. But don't worry, you don't have to return to Neanderthal cuisine now. It is quite enough to aim for a rough approximation of the primal diet.
So if you eat a lot of vegetables, salads and whole grains while avoiding meat, fatty foods and sweets, you are already on the right track.
Having treated many thousands of fibromyalgia patients so far, we can say that a certain type of dietary change is usually the most effective self-help measure.
You can find the background, diet and recipes in the download section. You will also find this detailed in several books.
Study
There are few studies on the subject of fibromyalgia and nutrition. However, a Finnish study points in the right direction.
Important: However, it does not depend on a strict vegetarian or even vegan lifestyle. Decisive is the question whether the gastro-intestinal tract is irritation-free or not.
Complaints can be reduced by consistent Diät and pain medicines reduced - that show results of a recently published study from Finland.
Already in earlier research studies the positive effect of a nourishing change with rheumatism tables illnesses could be proven. Since these investigations referred however almost exclusively to patients with rheumatism arthritis, now for the first time researchers of the University of Kuopio examined, which effects a veganen nutrition on the Symptomatik of Fibromyalgie patients has.
Over a 3-month period, 18 fibromyalgia patients underwent a strict low-salt diet consisting of uncooked vegan foods (berries & fruits, vegetables, mushrooms, seeds & nuts, legumes and grains). A control group of 15 female patients, who did not differ from the first group in age, height, weight, and severity of symptoms, maintained their original dietary habits. All subjects met the 1990 ACR fibromyalgia criteria. Previous medications were taken unchanged, but pain medications were allowed to be dosed by the participants themselves.
At baseline, 66% of all fibromyalgia patients were overweight (body mass index in both groups = 28). While the weight of the control group remained stable with the same diet, the participants in the diet group lost a significant amount of weight. Urinary protein excretion also fell to one-third of baseline and serum cholesterol levels decreased considerably, demonstrating a good response to the dietary change. If both groups had still complained at the beginning about very strong pain in the rest condition, these could be clearly reduced with the Veganern during the 3-monatigen Diätphase, which made a reduction of the pain means possible around up to 50%.
Significant changes could also be observed in other parameters: the patients reported an improvement in sleep quality and general health, as well as a reduction in morning limb stiffness. The participants in the diet group achieved better results in the general health questionnaire and in the special rheumatological questionnaire. Only the number of tender points showed a slight positive trend.
After the end of the research study, all subjects were allowed to eat according to their wishes again, with the result that the majority fell back into old habits and most laboratory values returned to the level before the diet began.
Source: Kati Kaartinen et al, Vegan diet alleviates fibromyalgia symptoms, Scand, J. Rheumatol. 2000, 29, 308-13.
Massages - better than your reputation
Classic massages have not proven effective for fibromyalgia. Especially the kneading massage worsens the complaints considerably. The harder the massage, the worse the symptoms!
More favorable are gentle stroking massages, which soothe, relax and reassure. Our patients and also we are very convinced of the effectiveness of this method, which we use in many ways.
We have equally positive experience with lymphatic drainage (e.g. in the form of manual lymphatic drainage). However, this form of therapy requires special training. You should inquire whether your therapist has this additional training.
In recent years, we have been using vacuum massage with great success, in which the skin is not pressed but, on the contrary, lifted. This can be done in the classical form with a cupping glass or - better - in the form of a pulsating vacuum with the help of an appropriate device. Almost all patients report significant relief after such treatment. The principle of the treatment is a drainage of the congested lymph from the depth of the connective tissue through the lymphatic channels. As a result, the muscles and connective tissue are decongested and automatically loosen up.
It is essential that massages are only a part of a larger - multimodal - concept, which also includes a certain hardening.
Heat and cold
Infrared cabin(IRK) is an effective method of heat treatment. Externally, it resembles the Finnish sauna. However, unlike the classic sauna, there is no stove that heats the air. In its place there is a combination of surface and point radiators, whose mild heat acts directly on the body. The IRK in our practice is made of untreated cedar wood and is therefore very suitable for allergy sufferers.
- The temperature of the IRK is very pleasant 40° to 60°C.
- You do not have to sweat to achieve an effect.
- Due to the deep effect of the infrared radiation, muscles, tendons and connective tissue are sustainably heated up to the lower tissue layers.
- You can also enter the IRK with (light) clothing.
- If you prefer, you can even leave the door open without loss of effect. This is especially pleasant for people for whom it is easy to get "too tight".
Whole-body cryotherapy is a highly effective therapy for various rheumatic diseases, originally developed in Japan and known in Europe since 1980. In Germany it was introduced in 1985 in various clinics (mainly rheumatism clinics). Since 1998, it has been possible for the first time to perform this therapy on an outpatient basis. We were the outpatient pioneers of this therapy in Germany.
The cold chamber is a room of about two to four square meters, which is cooled to a temperature between -70 and -80°C. The air circulation is very important. In addition to the temperature, the air circulation can be regulated so that the heat extraction from the skin can be customized. In this way, the subjectively effective temperature (wind chill) can be lowered to over -100°.
Physiotherapy
Anyone who has been able to move only with pain for a long time often finds that their muscles shorten and movements become painful and inharmonious. Targeted physiotherapy provides a remedy here. As part of our intensive therapy program, we perform it every other day or even daily.
Vibration plate
Fibromyalgia patients experience one thing in particular during physical training: pain, pain and more pain! And this either immediately during the load or - even more frequently - at night and the day after.
Nevertheless, muscle building is sensible and necessary. Especially if this is combined with muscle relaxation.
We carry out special training with the Galileo system in our practice clinic. It is a scientifically excellent studied system, with which you can build up the muscles in a very effective way , improve coordination, loosen muscles, strengthen the pelvic floor and the back muscles.
This form of training is also excellent for severely impaired pain patients.
Weightless running
AlterG is a new type of training device used in medicine and sports rehabilitation. It is a computer-controlled treadmill system on which the body weight can be reduced to almost zero gravity.
The name is derived from "to alter" = to change and "G" the name for gravity ("Gravity"). It is therefore possible with AlterG to reduce one's own gravity.
The technology was originally developed by NASA to study the training of astronauts under suspended gravity. It was recognized that training under reduced gravity could be used to great benefit in the rehabilitation of patients.
And the soul?
Not all complaints have physical causes. The human soul also plays a role in their development that should not be underestimated: stress, overwork, human conflicts in the family or at the workplace can contribute to the development of many diseases: in part, they aggravate already existing diseases, in part they cause them in the first place.
As a common denominator, it can often be found that increased emotional vulnerability also leads to increased physical sensitivity. A fact that has nothing to do with "imagination", but is to be understood as an adaptation reaction of the body to a real or experienced threat from the outside.
Often the roots of increased vulnerability reach far back into childhood. For example, we find that in many people who suffer from chronic pain, (early) childhood was unfavorable: insecurity, lack of security or injuries are often found.
Since nothing is harder to bear than an unknown threat, children often react by developing a heightened sensitivity. They try by all means to grasp the threatening environment as quickly and accurately as possible in order to adjust to the dangers.
The heightened sensitivity can be a gift. It can lead to sensitivity, deep resonance with others, and a high degree of empathy.
On the other hand, people with heightened sensitivity also suffer more often from increased self-awareness. They perceive the body, internal organs, pain but also, for example, light, noise and smell more clearly than others.
Psychotherapeutic procedures are therefore a further offer for our patients. Often no long-term therapies are necessary here, but a few conversations are sufficient.
In addition, relaxation procedures and sleep hygiene are important building blocks for raising the stimulus threshold again.
Pension & Co
Incapacity to work
Fibromyalgia often causes such severe discomfort and fatigue that it is temporarily impossible to work. Then it makes sense to stay at home for a few days to recover. However, if the impairment is more severe, it is important to remember that the symptoms will not resolve on their own. While a flu is cleared up after 14 days even without therapy, simply waiting does not usually help with fibromyalgia. Then valuable time goes into the country and sometime six weeks are past, in which the employer continues to pay the wage.
Therefore, in the case of fibromyalgia, the period of incapacity for work should be actively used for therapy, which you do not have time for in your everyday working life. Once again, resting is only helpful in the very short term!
Another thing you should keep in mind: The longer the disability lasts, the more difficult it is for most people to return to work. These difficulties should not be confused with the symptom "fibromyalgia". It is simply "withdrawal from work." In a mild form, you may know it after a long vacation.
Sick pay
Following this period, the health insurance fund steps in with sick pay. This is paid over a period of 78 weeks. The period begins with the first day of illness due to a specific illness within a period of three years. If you are sick for less than 78 weeks for three years because of the same illness, you are again entitled to 78 weeks of sick pay.
Rehab before pension
In Germany, the sensible principle is that "rehab comes before pension. Before someone is threatened with retirement, everything humanly possible should therefore be done to achieve an improvement or prevent a deterioration. If this is possible, the insured person has a duty to cooperate in medical rehab.
Application forms are available from the provider of the rehab measure (health insurance funds, LVA, BfA). Part of the application is generally a form for the doctor, in which he/she enters the type of illness and the reason for the rehab. Here the family doctor and also you yourself can make suggestions for a clinic.
Pension application
If, due to an illness, the ability to work or earn a living cannot be restored and rehabilitation has not been successful, a pension is generally paid in Germany.
Before applying for a pension, one should check whether the prerequisites (e.g. contribution periods) for this are met and whether a pension makes economic sense. After all, once a pension has been granted, other benefits such as sick pay or unemployment benefits are discontinued. You can then no longer withdraw from the pension just because you are worse off.
A pension application takes time! This period of time should be taken into consideration, because during this time the entitlement to certain social benefits may expire. The best thing to do is to contact the relevant pension insurance information office and have the presumed pension calculated.
Many affected persons seek advice from theVdK.
The application for a pension is submitted to the competent pension institution (LVA, BfA, professional pension institution, etc.) or to various other offices. You will receive numerous forms that have to be filled out. Medical reports or certificates are not necessary at this point. In most cases, the forms ask for the attending physicians. Depending on the individual case, the insurer will then write to them and request a form report or a longer report. In most cases, the pension insurance will appoint one or more experts who will then carry out examinations.
Based on these documents, a decision is made on the pension application.
File
The pension office decides on the basis of the files. As a rule, there is no personal examination. Often, a handful of medical experts have to judge the applications of tens of thousands of sick people year after year. It is easy to understand that under such conditions it is difficult to decide fairly in every case.
Again, the quality of the assessment depends crucially on the documents and certificates submitted. The above-mentioned criteria for a medical assessment apply here just as they do for the pension application. However, such a differentiated assessment represents a high effort, which is unfortunately only reimbursed to the treating physician with a very small amount.
The pension office determines a degree of disability in steps of 10 on the basis of the files. If there are several functional impairments, these are assessed individually and an overall degree of disability is fixed at the end. The last step is not simply added up, as is often assumed.
One usually starts with the disease with the highest degree of disability and then checks whether there are other functional impairments that cause a GdB of 10 or more. If the diseases are independent of each other in their effects, an increase of the total GdB will result. However, if they largely overlap in their effects, then even significant health impairments will increase the total GdB little or not at all. Similarly, minor limitations with an individual GdB of 10 do not usually increase the overall GdB.
Thus, if someone can no longer walk due to illness and a GdB has already been determined for this, then another illness that affects walking will not increase the overall GdB.
GdB for fibromyalgia - comparisons with other diseases
Fibromyalgia is listed in the "indications" following the inflammatory rheumatic diseases: "Also in the assessment of non-inflammatory diseases of the soft tissues (...so-called fibromyalgia syndrome), the type and extent of the respective organ involvement as well as the effects on the general condition are important."
Essential for a correct estimation is therefore the extent on the general condition and this must be explained in the individual case. If this is neglected and only the diagnosis is communicated, the pension office will routinely come to a rather low rating of 10-20.
If one would like to arrive at a higher rating, especially in the case of a dispute, a comparison with other diseases must be used in addition to a differentiated assessment of the "impact on everyday life", which are presented in a more differentiated manner and with percentages in the "indications".
The following diseases are conceivable:
- Inflammatory rheumatic diseases
- Migraine
- Facial neuralgia (e.g. trigeminal neuralgia)
- Neuroses and psychovegetative complaints
- Tinnitus (ringing in the ears)
- lymphedema
- chronic intestinal disorders (irritable bowel)
- muscular diseases and others.
Which comparison is used in each individual case depends on the assessment of the evaluating physician and the nature of the disease. The psychological consequences and accompanying symptoms of fibromyalgia should not be placed too far in the background. The depressiveness that accompanies the disease is often a significant reason for a higher GdB.
It is also possible that sometimes instead of the diagnosis "fibromyalgia" (M79.70 according to ICD 10) rather the diagnosis "persistent somatoform disorder" or "somatoform pain disorder" (F45.4 according to ICD 10) is made. With this diagnosis it is assumed that the reasons for the pain lie in the mental area.
Objection, deterioration
If you do not agree with the decision of the pension office, you can file an appeal or a lawsuit. The legal procedure is the same as for pension issues. In addition, after a certain period of time, you can submit a new application due to a worsening of your symptoms.
Certificates and expert opinions

The medical assessment is of decisive importance in the procedure. This applies not only to the expert opinion in the narrower sense, but also to the certificates issued by general practitioners or specialists. Together, they provide the basis for the judge's decision. The fairness of their decision stands and falls with the quality of the medical assessments. If these are negligent or meaningless, the judge will hardly be able to make a proper decision.
As a general rule, the diagnosis of a disease means little with respect to the granting of a pension. It is not the nature of the disease that matters, but its practical effect in everyday life. Most diseases, up to and including cancer, can result in minor or even massive impairments. With regard to fibromyalgia, additional difficulties arise because this diagnosis is controversial and difficult to objectify.
Thus, if a certificate from the family doctor simply states the diagnosis "fibromyalgia", this can never be the basis for a pension. If the affected person assumes that the judge must have an idea of the extent of the complaints, then he will feel deeply misunderstood if the pension application is rejected.
Helpful, i.e. meaningful, are certificates and expert opinions that go into detail about the specific symptoms and their effects in everyday life.
Example of useful certificate
History
- Beginning of the pain disorder
- Development of the complaints
- Type, extent and success of previous medicinal, physiotherapeutic/physical, inpatient, rehabilitative and psychotherapeutic treatments
- Possible own efforts or treatments by alternative practitioners
- Frequency of change of physician or therapist
- Type, extent and success of current therapy (medication, physiotherapy/physical measures, psychotherapy, etc.)
- Other diseases
Type of pain
- Intensity of the pain (pain scales)
- Location of the pain
- Type of pain (burning, drilling, stabbing, shooting in, etc.)
- Frequency of the pain
- Dependence of pain on external factors (weather, season, activity, especially occupation.)
Functional complaints
- Sleep disturbances
- Respiratory problems
- Palpitations and heart palpitations
- Irritable bladder
- Period pain
- Numbness
- Tremor
- Lumpy feeling in the throat
- Gastrointestinal disorders
- sweating, freezing
- Dizziness, lightheadedness
- Edema
- Sexual disorders
General performance
- Fatigue
- Fatigue
- Lack of rest due to nocturnal sleep
- Lack of concentration
- Decrease in mental performance
Mental complaints
- Depression
- Anxiety/phobia
Effects of the complaints on everyday life
- Work
- Daily routine
- Household
- Leisure time
- Hobbies
- Vacation
- Car trips
- Sports
- Relationships
- Social integration
- Sexuality
Examination findings
- General physical findings
- Musculoskeletal findings
- Strength
- Movement restrictions
- Neutral zero method
- Hand and foot calluses
- Indications of physical activity .
- Muscle sheathing of the extremities, training condition
- Presence of tender points
- Psych. findings
- Psychological tests, if applicable
Additional findings
- Laboratory (exclusion of inflammatory diseases, hormone determinations, etc.)
- Functional examinations (Schellong, ergometry with lactate determination, etc. depending on the individual case and possibilities)
Diagnoses according to ICD
- For example: "Fibromyalgia syndrome (M79.70)".
- If applicable, statement and summary of the most important data and a critical appraisal of their impact on work and everyday life.
If a physician's report comments in this way, it gives a court an informed basis for a decision. Whenever possible, physician and patient should collaborate on such qualified reports, although they also require significantly more effort.
If you need an expert opinion
Patients frequently contact us in order to obtain a new expert opinion. Often the experience is based on the fact that neither the orthopedic, psychiatric or neurological expert opinion has sufficiently evaluated the pain symptoms.
If you would like us to prepare an expert opinion, the following procedure is recommended:
You are welcome to ask us about the time frame in which we can prepare an expert opinion. Then talk to your legal representative (e.g. lawyer, pension representative or VdK) so that he can inform the court that we will prepare an expert opinion according to §109. This paragraph states that you have the right to appoint an expert yourself. However, you or your legal protection insurance must bear the costs. If the expert opinion reveals new, significant aspects, the court may decide to pay the costs afterwards.
We then receive the court documents and arrange an appointment with you for the examination.
We do not prepare private expert opinions without a court order, as this usually only causes unnecessary costs.
Videos personal reports
Books

There are numerous books available on the subject of fibromylagia.