Up to 25% of women of childbearing age suffer from chronic pelvic pain. For men, this percentage is somewhat lower.
There are numerous organs in the pelvis in a confined space: bladder, urethra, rectum, vagina, etc. All organs can become inflamed by bacteria, for example, causing clearly defined and distinguishable clinical pictures.
But there are pains that are far less well describable, but are nonetheless agonizing. These are chronic symptoms with little tendency to improve, which can originate in various organs and lead to a similar clinical picture known as chronic urogenital pain or "chronic pelvic pain".
Complaints
Typical symptoms
- Pain for more than 6 months
- Often diffuse and difficult to localize
- Pain character: from dull-pulling to stabbing
- Duration of pain: from short cramps to constant pain
- Pressure and heaviness in the pelvis
- Discomfort during urination
- discomfort during intercourse
- Irritable bowel complaints: Constipation, diarrhea, flatulence, pain
- Sleep disturbances, anxiety, depressive moods
- General hypersensitivity
Almost all patients report that
- the usual treatments (from medication to surgery) are of little or no help.
- an organic cause for the complaints had not been found, although they had been diagnosed again and again
- they are very impaired in their mental well-being
- they are also restricted in their general activities
- the partnership is also affected by the complaints.
Trigger
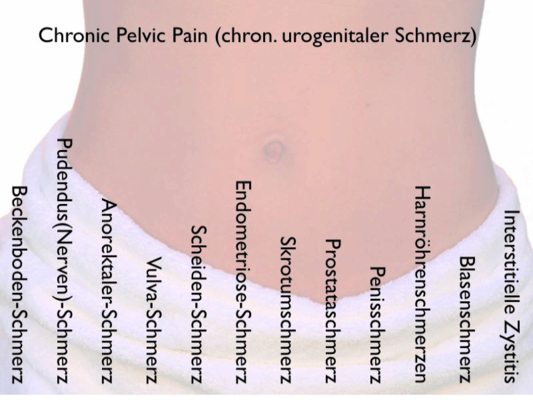
Endometriosis
The endometrium is the inner mucous membrane of the uterus (womb). However, this mucosa can be found in the form of "islands" in other parts of the body. Most often it is the abdominal cavity, especially the pelvis. However, at one time it may also be a distant organ such as the lungs. These mucosal islands grow and shrink in rhythm with the female cycle.
Endometriosis is common. Approximately 10% of all women of childbearing age are affected. The size of the endometrial islets varies from lentil size to orange size. After menopause (menopause), the symptoms subside.
Endometriosis often triggers increased menstrual pain. In addition to abdominal pain, pain in the back or pain during intercourse are common. There is no fixed relationship between the number and size and the discomfort. On the contrary, during a laparoscopy, numerous endometrial foci are often found in women who have no complaints at all. But there is also the reverse case: severe pain with few findings. It is discussed whether water retention in the abdominal cavity can aggravate the symptoms.
Therapy is either medicinal (e.g. hormones) or surgical. Complete removal of all endometrial foci is often not possible.
Adhesions, scars
Adhesions are scars in the connective tissue of the abdominal cavity. They can form, for example, following abdominal surgery (inflammation) between internal organs. Usually they do not cause any discomfort. However, they may cause pain or cramps - in case of unfavorable location or increased sensitivity.
In rare cases, the intestine can become completely strangulated. This results in intestinal obstruction (ileus), which must be surgically removed.
However, the question always arises as to whether adhesions are actually the cause of the discomfort or whether adhesions are only found by chance in people with abdominal pain. In an English study, no differences were found in 100 women with and without adhesions with regard to this symptomatology. Apparently, the pain has other causes.
Vestibulitis
Vestibulitis or focal vulvitis is an extremely painful inflammation of the external genital organs of women (labia minora, labia majora, clitoris, vaginal vestibule). The vaginal vestibule is often reddened. Even minimal touch triggers a sharp pain. Riding a bicycle, wearing tight pants or even intercourse are not possible.
The cause is unclear. Frequent infections occur in the history, but are not the only triggers.
Therapy is difficult, often not successful. More commonly, the hypersensitive tissue is surgically and extensively removed.
Interstitial cystitis
This is a chronic inflammation of the bladder that is not caused by bacteria. One finds a disturbed structure of the bladder mucosa, which is more permeable to harmful substances.
In the course of the disease, there is a hardening (fibrosis) of the bladder wall and increasing shrinkage.
The main symptoms are a constant urge to urinate, which can be particularly agonizing at night, and pain. Sufferers have to go to the toilet up to 60 times a day.
A clear cause cannot be identified. Therapy is difficult.
Chronic prostatitis
Following acute prostatitis, i.e. bacterial inflammation of the prostate with fever and severe pain, chronic complaints may develop without pathogens being identifiable.
These complaints then moderate into a chronic pain syndrome that is almost indistinguishable from other forms of urogenital pain. Again, therapy with antibiotics/pain medications is usually not very successful.
Irritable bowel
For this we may refer to the extensive presentation on this page.
Abdominal pain is very often associated with irritable bowel syndrome. In a study of 798 women with abdominal pain, half also had IBS.
Sleep disorders Depression Anxiety
Chronic sleep disorders, depressive moods and anxiety are also risk factors that promote abdominal pain, but the relationship here is different from the conditions listed above.
These medical conditions lower the stimulus threshold in a non-specific way, i.e. they make people more "sensitive", which has nothing to do with imagination.
A high risk for abdominal pain is also borne by those who have suffered sexual abuse either in childhood or as adults. The explanation for this is obvious.
Causes
Local hypersensitivity - peripheral sensitization.
At the beginning of chronic complaints there is usually a local pain, e.g. acute prostatitis, vaginal mycosis, inflammation of the vulva, bladder infections or disorders of the rectum.
If this pain persists for a long time, local sensitization occurs. The tissue becomes hypersensitive. This is a process that is very common in chronic irritations.
Sensitization is particularly pronounced when irritation is present at multiple sites in the abdomen. In an American study on rats, it was found that the so-called visceral nerves are particularly irritated when several types of complaints are present at the same time. ( Ethn. dis. 2008 Spring;18(2 Suppl 2):S2-20-4)
That is, if irritable bowel syndrome is present at the same time, then chronic cystitis, for example, will have a much greater effect.
Pain amplification
In addition to these local stimuli, however, there are non-specific amplification mechanisms: these are primarily anxiety, depression, sleep disturbances, and chronic stress. All of these factors increase sensitivity in general.
Thus, if pain is associated with strong anxiety or with apprehension, it will be perceived more strongly.
Central hypersensitivity - central sensitization
As this progresses, a process best described as "central sensitization" sets in. What is meant by this is the following:
Our brain has to deal incessantly with the influx of signals from the body. There are probably several dozen million sensors in the body that send signals to the brain on a more or less regular basis. If we were to perceive all this at the same time, we would be hopelessly overwhelmed.
So the brain "fights back" and sends dampening signals to the spinal cord and peripheral nerves to limit the flood of information while allowing only the most important impulses to pass through.
Continuous pain - no matter from which region - has the property to exhaust this damping ability.
Everyone knows this phenomenon from everyday life. If you are forced to do concentrated work in a noisy environment, you will only succeed for a limited time. At some point, one is no longer able to block out the ambient noise. One can also say that the stimulus threshold has dropped, and the same noise level is perceived as much more unpleasant.
This is also the case with chronic pain. If it lasts for a long time, the stimulus threshold decreases and we perceive the disturbing signal as more painful than at the beginning.
Self-reinforcing vicious circle
If the discomfort lasts for a long time, a vicious circle can develop. Continuous pain lowers the pain threshold and this leads to the influx of more pain signals.
It is almost like a boat with a list. The more severe it is, the more water flows in. The water, in turn, reinforces the listlessness....
As a rule, those affected can no longer get out of this vicious circle under their own steam.

Therapy
If one reads the literature on the therapy of chronic abdominal pain, one quickly finds a commonality: the pain is considered to be extremely difficult to treat. Whether chronic prostatitis, vulvodynia, vestibulitis or irritable bladder - all diseases are considered therapeutically "ungrateful".
As with other functional complaints
The reason is comparatively simple. The complaints are not (or only to a small extent) caused by a change in the local tissue. The actual cause lies in the change of the peripheral and/or central stimulus threshold. The result is excessive sensitization, i.e. real (not imagined) hypersensitivity of the corresponding region.
This type of change can be seen poorly or not at all on physical examination, they do not present themselves on X-ray, ultrasound or laboratory tests.
Accordingly, even local treatments rarely bring about an improvement, which is frustrating for doctors and patients alike.
All too often, the medical profession tends to attribute the symptoms, which do not seem to have a clear cause, solely to psychological factors. Those affected are advised to consult a psychotherapist or psychiatrist. If one merely receives medication there, e.g. antidepressants, this rarely changes anything about the pain. Sometimes the side effects are stronger than the symptom relief.
Of course, pain also has psychological causes. As mentioned, anxiety, inner tension, chronic stress or depression exacerbate a pain disorder. In this respect, it can be very useful to include psychotherapeutic elements in a more comprehensive treatment concept. However, psychotherapy alone and, in particular, exclusive treatment with antidepressants (drugs for depression) very rarely lead to success.
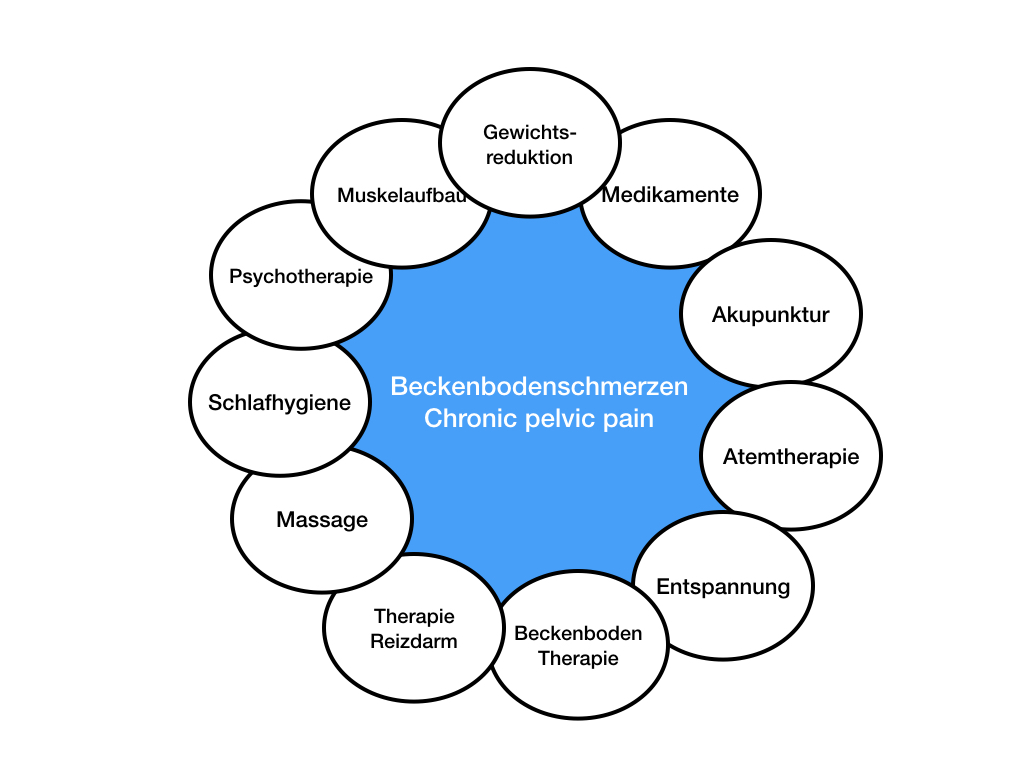
"Gold standard" multimodal therapy
Successful therapeutic strategies, however, take a somewhat different approach. An attempt is made to gradually raise the lowered stimulus threshold in order to achieve lasting freedom from symptoms. Especially multimodal (multi=many, modus=way) therapy methods are effective, which rely on more than one therapy method.
Dilemma
One of the great difficulties in the therapy of abdominal pain is that the obvious therapeutic procedures are largely ineffective, and may even aggravate the discomfort.
For example, if there is severe discomfort from vulvodynia or vestibulitis, then many local therapies will cause the discomfort to worsen. Treatment or diagnostic interventions only further lower the threshold of irritation, further exacerbating the pain.
This fact puts many sufferers in great perplexity as they wonder what else they can do. Often the perineal region is so painful that any touch - let alone treatment - causes pain.
Direct or perineal?
As shown above, most types of abdominal pain do not occur in complete isolation. They are often accompanied by other pains or conditions that contribute to or exacerbate them. For the person concerned, it is bad to have so many complaints. However, this fact can be used extremely productively for therapy.
If one suffers from several types of pain, (e.g. back pain and pain in the abdomen), one will notice that these pains often increase or decrease together.
It may be that one region (such as perineum/vulva/anus) is so extremely sensitized that any therapy here is impossible. In such cases, one will try to prioritize other pains first, such as back pain or intestinal discomfort.
If one succeeds in alleviating these other complaints, one is often surprised to find that the "actual" pain has also improved. In short, the pain thresholds in different areas are interconnected. Thus, apparent detours lead more quickly to the goal.
Multimodal therapy
In everyday clinical practice, there are usually more than two symptomatologies. Often there are numerous complaints from which the affected person suffers. The medical art is to treat the essential complaints in the right order. If a doctor prescribes too many or the wrong procedures, the symptoms will increase; if he prescribes too few or the wrong ones, they will not improve.
How a treatment is designed in detail depends on the individual case. However, experience shows that the quality of sleep, the condition of the gastrointestinal tract, the absence of muscle or joint pain, and the reduction of anxiety are essential elements of therapy in most cases.
Many sufferers complain of increased sensitivity to cold and/or heat. This usually has nothing to do with body weight, but with the lowered stimulus threshold for heat and cold stimuli. If the stimulus threshold can be raised (by alternating heat and cold therapy), this also has an effect on the pain threshold, and the general hypersensitivity decreases. A fact that used to be called "hardening" or "roborating".
Equally important: respiratory therapy. Here we almost always find abnormalities, especially in the form of accelerated, restless breathing. Also because of the close relationship between the pelvic floor and the diaphragm, which oppose each other as antagonists, respiratory therapy has a very beneficial effect here.
Duration
If the complaints have become chronic over a longer period of time, intensive treatments are often necessary in order to effectively break the vicious circle of pain. From our experience, 2-3 week treatments are useful in order to achieve significant therapeutic progress.
Depending on the possibilities, we then extend the therapy intervals or switch completely to self-help or therapy at the place of residence.