Exhaustion is first of all a completely normal feeling. If you have worked a lot or have been able to get little sleep, then you need not be surprised if you feel tired at some point. But that is not what is meant here: it is not a calm, contented tiredness, but a restless, driven exhaustion, a tension-filled emptiness.
Another difference: if you have simply done too much for a while, then a soothing night's rest, a relaxing weekend or, in a pinch, a few quiet vacation days or weeks will help.
But for patients, it's different. Neither the night sleep, nor the sick leave, nor the rest during the day somehow makes it better. They have an almost indomitable need for rest and recuperation - but that need cannot be satisfied. It seems like an evil curse: the more they rest, the more exhausted they feel. We have patients who, after months or years of rest, can practically only lie down. Even sitting overwhelms them after a short time, not to mention standing or other movement.
What kind of complaint is this? What is to be done?
Intro
Long Covid
Causes and treatment options of long Covid
Brain Fog
CFS - Chronic Fatigue Syndrome
CFS
More and more frequently, patients come to us complaining of more or less similar complaints. For a long time they were in the middle of life: Active, fully engaged in their profession and besides that also interested in many areas in their free time. Perhaps there was also stress and sometimes it all became too much for them. But somehow they always managed to get through it.
Then, however, a banal infection comes along, not unlike what they have often had in the past. They feel very miserable and battered, just like a "flu" brings. But instead of being over after a week or two at the latest, as is usually the case, the feeling of exhaustion and shattering remains.
Days, weeks and months go by - and it doesn't get any better. They feel tired, "flu-like," have muscle and joint pain, suffer from dizziness, lightheadedness, fatigue, difficulty concentrating, numerous so-called functional complaints, sensitivity to light and noise, and many other symptoms. Some patients report that they are forced to spend up to 18, 20 or even more hours in bed, up to 12 hours at night and then again during the day for many hours. But sleep does not bring the desired recovery, usually they feel worse when they get up than the night before.
In short: they are only a shadow of their former selves.
Typical complaints
CFS (Chronic Fatigue Syndrome) is an abnormal fatigability after physical or mental exertion that does not improve after rest.
Characteristic is:
-
Often an onset that can be named in time; frequently, affected persons can name a specific date. However, there are also patients who slowly slip into exhaustion.
-
No connection of a clear physical or mental overload, which would make the feeling of exhaustion understandable.
-
Long duration of symptomatology, i.e. longer than three (according to other authors: six) months
-
The physical and mental performance reduction (e.g. less than 50% of the initial level).
More symptoms
Contrary to what the name suggests, exhaustion makes up only part of CFS. The symptomatology by no means consists only of the feeling of fatigue and excessive demands.
In most cases, a host of other functional disorders is present. Thus the symptom picture resembles also other illnesses, which are represented on these sides. In particular, fibromyalgia syndrome, irritable bowel syndrome, various forms of sleep disorders, dizziness, feelings of weakness or functional disorders in general.
Also disorders of the immune system, especially the lymphatic system, are common.
Other complaints: headaches, sore throat, muscle and joint pain, concentration and memory disorders, non-restorative sleep, sensitivity of the lymph nodes, nerve twitching and tingling in the body, depression, ringing in the ears, visual disturbances, allergies, subfebrile temperatures as well as a persistent worsening of the condition after exertion and much more.
Diagnosis
Diagnosis
Decisive for the correct diagnosis are the conversation and the examination by an experienced physician.
He (or she) should be familiar with the corresponding organic as well as mental illnesses that come into question as differential diagnostics. This is followed by the normal physical examination, which also provides important information.
The clear diagnosis of CFS has not become easier due to the multitude of diagnoses. These different definitions ultimately try to describe a phenomenon that is still not understood. A2020 paper pointed out that a total of 25 definitions/descriptions have been used since the first description by Fukuda in 1986 to 2020! It is quite obvious that a multitude of different causes are hidden under the respective terminology.
- The core symptomatology is exhaustion, the lack of recovery through sleep and rest, and massive fatigue after exertion.
- Other signs of immunological reactions of the body, functional disorders, pain and psychological impairment are also present.
- Other diseases should be excluded.
Fukuda diagnosis
Main Criteria_ The diagnosis of "CFS" may be made when there is unexplained persistent or recurrent chronic fatigue,
-
of at least 6 months duration
-
with a new or clearly defined onset (does not already exist throughout life)
-
that is not the result of current stress
-
which is not substantially alleviated by rest/recovery periods
-
that results in a substantial reduction in occupational, educational, social, and personal activities compared to the period before the illness.
Secondary Criteria: Concurrent presence of 4 or more of the following symptoms for at least 6 months:
-
Memory and concentration problems
-
Sore throat
-
Sensitive/painful cervical or axillary lymph nodes
-
Muscle pain
-
Joint pain with exclusion of arthritic disease
-
Headaches of unknown type or intensity
-
non-restful sleep
-
Disproportionate fatigue after exertion lasting longer than 24 hours
Exclusion Criteria: The following medical conditions must not be present.
-
Demonstrable medical illness that may explain the symptomatology.
-
Prior demonstrable medical illness that cannot be clearly demonstrated but whose possible persistent activity could explain the symptomatology
-
Depression with psychotic, catatonic, or melancholic features; bipolar disorder (manic-depressive); schizophrenia and psychotic disorders; dementia; eating disorders
-
Alcohol, substance, or medication abuse or dependence within the 2 years prior to the onset of chronic fatigue, and at any time thereafter
-
Severe obesity (BMI greater than 45).
Diagnosis according to CDC criteria (Centers for Disease Control and Prevention 1988/1994)
Main criteria:
Initial onset of persistent or recurrent chronic fatigue not otherwise explainable that does not improve with rest, significantly interferes with lifestyle, and has persisted for at least 6 months.
Ancillary Criteria: At least 4 of the following concomitant symptoms (also of at least 6 months' duration) must be present:
- Impairment of short-term memory or concentration.
- Sore throat
- Pressure painful lymph nodes
- Muscle pain, multiple joint pain (without swelling or redness)
- New onset of headache
- Non-restful sleep
- Discomfort after physical (or mental) exertion lasting more than 24 hours
Exclusion criteria
- Fatigue symptoms that are medically justifiable in another way, e.g. hypothyroidism, sleep apnea, narcolepsy and side effects of medication
- Malignant diseases, hepatitis B or C
- Psychiatric disorders: Specifically, any diagnosis of prior or concomitant so-called endogenous depression; also mentioned are bipolar disorder, schizophrenia, delusional disorder, dementia, anorexia nervosa, or bulimia nervosa
- Alcohol or other substance abuse at the time of symptom onset or at any time thereafter
- Severe obesity (BMI > 45 kg/m2).
Diagnosis according to International Consensus Criteria (2011)
Main criteria:
Post-exertional debilitation ("post-exertional malaise"): rapid physical and/or mental exhaustibility in response to exertion, symptom amplification after exertion (e.g., flu-like symptoms), immediate or delayed debilitation after exertion, prolonged recovery time (24 h), decreased activity level (compared with premorbid state).
Ancillary criteria:One symptom of each of the two categories.
- Neurological disorders: neurocognitive (difficulties in information processing or with short-term memory), pain (headache or other localization), sleep disturbances, other complaints such as increased sensitivity to stimuli, muscle weakness, coordination disorders
- Immunological, gastrointestinal or urological disorders: flu-like symptoms, susceptibility to infections, drowsiness, irritable bowel syndrome, urge incontinence, food intolerances?, orthostasis problems, hypotension, shortness of breath, ?temperature regulation disorders
Exclusion criteria:
- Primary psychiatric illness, somatoform disorders, and substance abuse, as well as any other conditions that may explain the complaints after thorough history, physical examination, or laboratory findings
Diagnosis according to Institute of Medicine (IOM) - 2015
Main Criteria: All three criteria must be met:
- Inability to maintain premorbid level of activity (occupational, social, educational, or personal), 6 months of fatigue, no significant improvement with rest
- Discomfort after physical or mental exertion
- Non-restorative sleep
Secondary Criteria: At least one of the two criteria must be met:
- Cognitive disturbances
- Orthostasis problems
Exclusion criteria:
- Other physical or mental illness
Systemic Exertion Intolerance Disease (SEID)
Criteria for systemic stress intolerance disease
Necessary criteria
- A substantial reduction or impairment in the ability to engage in occupational, educational, social, or personal activities prior to illness that lasts longer than 6 months and is accompanied by fatigue, often profound, that is new or definite in onset (not lifelong), is not the result of sustained overexertion, and is not substantially relieved by rest.
- Postexertional (post-exertional) malaise.
- Unfreshing sleep
Supplemental Criteria (one of two):
- Cognitive impairment
- Orthostatic intolerance(POTS).
Differential diagnostics
Exhaustion in family practice
Exhaustion that does not improve after rest is, of course, a very common symptom. A variety of diseases can be responsible for it. This is true at least in theory. In fact - according to onestudy- in the everyday practice of a family doctor, there are very few diseases in which exhaustion is the main symptom.
- Depression
- Anemia
- Cancer
- Serious physical diseases
Depression is at the very forefront. All the others are significantly less common.
One study concludes, "About one in five patients who complain of fatigue to their primary care physician suffers from a depressive disorder. A history that targets mental health and psychosocial well-being is therefore of great importance. Our review shows that anemias, malignancies, and other serious somatic diseases are very rare in fatigued primary care patients. Their prevalence rates differ little from those of nonfatigued patients. Extensive investigations are not indicated when fatigue occurs as an isolated symptom without additional findings from the history or physical examination.
Degree of severity
CFS occurs in very different degrees of severity. Exhaustion cannot be measured like blood pressure. Therefore, one tries to distinguish the severity based on the symptoms (according to 1CC, 2011)
Mild form
All daily errands can be performed alone, including household chores, although with difficulty. Occupation is maintained.Leisure activities are already largely limited. Weekends are entirely devoted to recovery for the week.
Moderately severe form
Mobility is limited. Daily activities and household chores can only be carried out to a limited extent. Occupational activity is hardly possible. Sleep is poor, afternoon sleep of 1-2 hours duration is necessary.
Severe form
Only small tasks such as personal hygiene can be performed. Severe memory and concentration disorders. Leaving the home is difficult, only possible in a wheelchair.
Most severe form
Complete confinement to bed, practically no activities of one's own, extreme sensitivity to light and noise. Continuously severe symptoms at rest and on exertion; constantly bedridden; unable to care for self.
Severity according to Bell
| Points | Symptomatology |
|---|---|
| 100 | No symptoms; normal activity; work and stresses problem-free. |
| 90 | Under stress, slight discomfort; normal activity; work and stress problem-free. |
| 80 | At rest, mild discomfort that worsens with exertion; minimal activity limitations with exertion; strenuous all-day work with problems. |
| 70 | At rest, mild discomfort that worsens with exertion; activity is near 90% of usual; clear limitation of some daytime activities; all-day work with problems. |
| 60 | At rest, mild to moderate discomfort that worsens with exertion; activity is near 70-90% of usual, clearly identifiable limitation of daytime activity; unable to work full time with physical effort, but able to perform light full-time work with a flex schedule. |
| 50 | Moderate discomfort at rest, moderate to severe on exertion; activity reduced to 70% of usual; unable to perform more strenuous tasks; able to perform lighter tasks 4-5 hours a day; rest breaks needed. |
| 40 | Moderate discomfort at rest, moderate to severe on exertion; activity reduced to 50-70% of usual; not confined to home; unable to perform more strenuous tasks; able to perform lighter tasks 3-4 hours a day; rest breaks needed. |
| 30 | At rest, moderate to severe symptoms, severe discomfort on all exertions; activity reduced to 50% of usual; confined mainly to home; unable to perform any strenuous duties; able to perform light tasks 2-3 hours a day; rest breaks needed. |
| 20 | At rest, moderate to severe symptoms; severe discomfort with all efforts; activity reduced to 30-50% of usual; rarely able to leave the house; in bed most of the day; unable to perform more strenuous activities. |
| 10 | Severe symptoms at rest and on all efforts; unable to leave home; bedridden most of the time; cognitive symptoms prevent concentration. |
| 0 | Continuously severe symptoms at rest and during exertion; constantly bedridden; unable to care for self. |
Facts Facts Facts
Frequency and gender ratio
To correctly estimate the exact incidence of CFS is problematic, because the diagnosis is very often made late or not at all. The disease is simply not diagnosed.
In the USA it is assumed that 1.7 to 3.3 million people are affected and a rate of 857 per 100,000 inhabitants.
Transferred to Germany this would mean about 600,000 patients with CFS. For comparison: That would be 50% more than sufferers of multiple sclerosis. Thus CFS would not be a rare disease.
But these figures are not undisputed. Otherauthors assume significantly lower frequencies.
Gender ratio
As always with functional disorders, women are more often affected than men. In the USA, however, 35-40% were also men.
However, there are errors here. Physicians apparently tend to diagnose such disorders more in women.
Symptoms
The fatigue is often hard to describe for those affected: "When I get up in the morning, I feel as if a steamroller had run over me during the night," reports one young man. "I then try to struggle out of bed and only after ages do I then come out and need 2, 3 hours until I can keep my eyes open to some extent.
After 2 hours, when I have expended just a little energy, I am then so exhausted again that I have to lie down again, although I have done almost nothing. I can't run my household, can't concentrate, can't do any physical work. I just shuttle between bed and armchair and can't get myself up to do anything."
The exhaustion increases thereby above all with physical in addition, with mental exertion, and/or after infections clearly.
Investigations showed that despite the complained forgetfulness, the intelligence is completely preserved. However, the mental performance was reduced in CFS patients. Above all, the speed with which certain tasks could be solved was lower than in healthy people.
Muscle pain
Besides fatigue, muscle pain is a major symptom (about 75% are affected). This is similar to sore muscles or as during a viral infection. One feels "flu-like" all the time.
Muscle fasciculations, the twitching of individual muscle bundles, is also a common symptom that can be very irritating for those affected.
The discomfort worsens with any form of physical exertion. This fact is significant, as it makes the frequently recommended sport practically impossible.
The pain is similar to that of fibromyalgia.
Alcohol, cigarettes, drugs?
In medicine, there is a tendency to associate numerous diseases with the usual suspect life circumstances (alcohol, smoking, obesity). But in the case of CFS, things look quite different. ADutch studyeven comes to a contrary conclusion: the affected people live significantly healthier!
"Compared to the general Dutch population, significantly fewer CFS patients were overweight. Significantly more female CFS patients abstained from alcohol, and fewer male CFS patients smoked. Unhealthy lifestyle factors were not significantly associated with fatigue severity or functional impairment."
Stress
Many patients report a stressful, hectic time before the onset of the disease. This is described as particularly stressful if other complaints such as infections, pain or stressful events such as separations or illness in the environment are added.
Another indication of the importance of chronic stress is the fact that natural disasters, violent events or severe emotional stress increase the chance of developing exhaustion.
Depression and anxiety
The soul probably plays a greater role in the development of fibromyalgia syndrome. In 50-80% of patients, there is a history of a more or less pronounced mental illness.
Especially depressive disorders are frequently present. A distinction between depression and CFS is therefore sometimes difficult, since depression is associated with exhaustion. Strictly speaking, depression is an exclusion criterion for CFS if it was already present before.
Subjective theory of disease
ADutch study investigated the so-called "disease attribution", i.e. to which causes the symptoms are attributed. It was found that patients who suspected external causes had more complaints. Possible explanation: They felt more helpless, more like victims.
Quote: CFS patients attributed their fatigue more often to external causes, reported poorer physical functioning, more doctor visits, and lower employment rates. Results of a regression analysis showed that patients who believe their fatigue is associated with more severe consequences, that their fatigue lasts longer, and is responsible for more additional symptoms are more likely to be classified as CFS, while patients who are more physically active and have higher levels of "all-or-nothing" behavior are less likely to be classified as CFS.
Hormonal changes
Corticotropin (CRH) is the central stress hormone and ensures the body's readiness reaction for flight and fight. Via the intermediate station of the pituitary gland (production of ACTH), cortisone is increasingly produced. This then ensures readiness.
However, permanent stress and permanent pain change the way the system reacts. Patients suffering from chronic fatigue appear to have lower blood cortisol levels and altered responsiveness of the CRH-ACTH-cortisone axis.
Growth hormone: Many studies suggest that low levels of growth hormone (GH) are both a consequence of the disease (lower production in sleep disorders) and play a role in causing the disease.
Melatonin: There are different results here, ranging from no difference to healthy individuals to increased melatonin production at night.
Sleep disorders
Sleep disorders are an essential part of CFS. In this case, those affected suffer from "hypersomnia," or an abnormal need for sleep. "I could sleep 24 hours a day without being well-rested, said one patient.
The hallmark is disturbed deep sleep, which is described as non-restorative sleep.
Anobjectification of the sleep disturbancesdoes not succeed however also in the Polysomnographie (sleep laboratory) usually. The sleep architecture is usually normal. Therefore, this lack of recovery is often interpreted as a misinterpretation of sleep.
Recently, we are increasingly studying the influence of carbon dioxide on sleep quality in CFS. This metric is usually not monitored in the sleep laboratory. It may play a major role regarding the restfulness of sleep.
Drowsiness and brainfog
Very many sufferers complain of a constant feeling of dizziness. They feel as if their head is wrapped in absorbent cotton or they have drunk too much. Not infrequently, they complain of a feeling of derealization, as if they were standing behind a glass wall and were not "really there".
This symptomatology is very similar to PPD, "vertigo without findings" or brainfog, which is explained in detail elsewhere.
Viral infections
Even though very many affected persons report a severe infection as the beginning of the symptomatology, the role of chronic viral infections in the further course is unclear.
Frequently, EBV infection is referred to as a possible cause. But it must be taken into account that the infectivity in the population is95%and the rate of CFS is less than 1%.
- Some subsets of white blood cells (B- CD19- lymphocytes) are increased, others (T- CD4- cells, T- CD8- cells) are decreased.
- The ratio between certain parts of lymphocytes is altered (T-CD4/T-CD8 ratio decreased).
- The number of killer cells is increased.
- Immunoglobulins show no clear findings (increase/decrease).
- Partial ANA (antinuclear antibodies) and autoantibodies are elevated.
Numerous viruses have been blamed for CFS. In CFS, signs of an infection that has passed through were indeed found to be disproportionately frequent. Whether this was actually the cause of the disease or just one of many triggers remains open. Personally, I tend to the latter view.
- Paroviruses: No clear connection
- Herpes Simplex Virus: No clear connection
- Cytomegalovirus: No clear connection, since most people had a contact anyway.
- Epstein-Barr virus (EBV): 90% of all adults have had contact with the virus. Certainly no "chronic EBV infection" is present.
- Human herpes viruses 6- 8: No clear connection
- Influenza viruses (flu): No clear association
However, the significance of these findings is open. Onereview concludes:
"Currently available data on the role of chronic viral infection in ME/CFS remain controversial; at least for a subset of ME/CFS patients, they show potential viral involvement."
Immunological changes
We consider immunological disorders to be very significant: Especially after physical or mental stress, there is a general feeling of illness or "flu feeling" with swelling of the lymph nodes or increased temperature.
Inflammatory factors in CFS have been reliably proven. Areview showed that patients with CFS had significantly elevated tumor necrosis factor, interleukin-2, interleukin-4, transforming growth factor, and C-reactive protein. Likewise, impaired T-cell metabolism wasfound, as was a reduction inco-enzyme Q10.
In aNorwegian study, CFS was treated with rituximab, which is otherwise used in cancer therapy and suppresses the immune system. After initial hope, further studies showed that this hope was premature. The side-effect-rich and expensive drug showed no improvement in symptoms within 24 months. On the contrary, the placebo group showed a better response (36%) than those treated with rituximab (26%).
It is unclear whether immunological changes are the actual cause or only the consequence of the symptoms (e.g. overstimulation of the immune system after a severe infection).
Changes in the mitochondria
Mitochondria are often referred to as the "power plants" of cells. They are the site for the citrate cycle and the respiratory chain. Therefore, more of these cell organelles are found in cells with a high energy turnover, e.g. muscle cells, sensory cells or nerve cells.
So could it be that the perceived lack of energy in CFS is due to a disturbance of these energy supplying cells? At least, this assumption does not seem unreasonable at first glance.
Mitochondriopathy: Diseases of the mitochondria(mitochondriopathy) are rare (about 12/100,000) and usually occur in childhood or early adulthood. There are several dozen known disorders. Diagnosis (usually muscle biopsy) should be done at aspecialized facility. Currently, there is no causative therapy and no cure. Various vitamins are used, but the effect is uncertain. Endurance training below maximum load, on the other hand, is recommended.
Pseudoscientific definition: The so-called "mitochondrial medicine" must be sharply distinguished from these serious diseases. It is a non-scientific model of thinking that associates countless disorders and diseases with a presumed disorder of the mitochondria. Therapeutically, a variety of vitamins and minerals are usually recommended.
CFS and changes in mitochondria: There are a number of scientific studies investigating the link between CFS and changes in mitochondria. The assumption that changes in energy production are responsible for the perceived exhaustibility is in some ways obvious.
However, such studies are by no means trivial, as the small power plants have a complex structure and numerous functions. The results of investigations are contradictory. Sometimes changes are found, sometimes not. However, the quality of the studies is highly variable. Was there a comparison group? Was age taken into account? How many people are included? How is the disease defined?
In 2020, acomprehensive comparative studyhas now beenpublished, highlighting 19 high-quality studies from the plethora of publications. Here is the authors' conclusion:
"Detection of potentially disrupted mitochondrial pathways is difficult to establish with certainty because of the use of different sampling methods. There is consistent genomic research suggesting that ME/CFS/SEID is not a primary mitochondrial disorder, but mitochondrial damage could occur due to secondary effects of other disrupted pathways. In addition, the findings were inconsistent across studies. Because the population samples were small, these findings should be interpreted with caution. The cause of ME/CFS/SEID remains unknown, and future studies using the same diagnostic criteria and analytical methods for ME/CFS/SEID are needed to determine the mitochondrial contribution to the pathomechanisms of ME/CFS/SEID."
CONCLUSION: There is a preponderance of evidence that the cause of CFS is not due to mitochondrial damage. This is also supported by the fact that corresponding therapeutic approaches with vitamins and enzymes usually do not show a pervasive and stable effect.
Inflammatory processes in the brain
A positron emission tomography (PET)scan found evidence of inflammatory processes in the brain that correlated with symptom severity.
Breathing and exhaustion video
Exhaustion and breathing disorders
From our point of view, very significant arestudies on shortness of breath in CFS, which are in line with our own observations. In one study, 54% of CFS patients but only 3% of controls showed relevant dyspnea. In contrast, lung function itself was not different.
This substantial difference suggests the importance of functional breathing disorders in CFS.
More in the presentations infunctional breathing disordersand their influence on cerebral blood flow.
There is a great deal of evidence, both in our patients with CFS and in theliterature, of impairedcirculatory regulation in CFS. Many of those affected fulfill the criterion ofpostural tachycardia (POTS), which, like CFS, is often accompanied by massive exhaustion.
Long Covid
Disease progression
Disease progression
The prognosis of CFS is a serious condition when fully developed. Many sufferers do not regain their full ability to perform.
1st cure: A smaller group that becomes completely symptom-free. However, it can take a long time before this happens. The percentage is 5% with wide variations depending on the study (0-31%).
2. fluctuating: those affected show an alternation of good and bad phases - 39.5% (range 8-63%).
3. deterioration: a small group becomes so severely ill that they remain confined to home, bed or wheelchair.
Indications ofbetter prognosis: rapid recovery after a bad episode, feeling in control of their own discomfort.
Indicationsof worse prognosis: complaints lasting longer than 5 years. Attribution of complaints to a physical cause.
Of course, thesefigures from 2005 do not take into account that progress in understanding has been made in the meantime and at least some therapeutic progress has been achieved.
Therapy
video
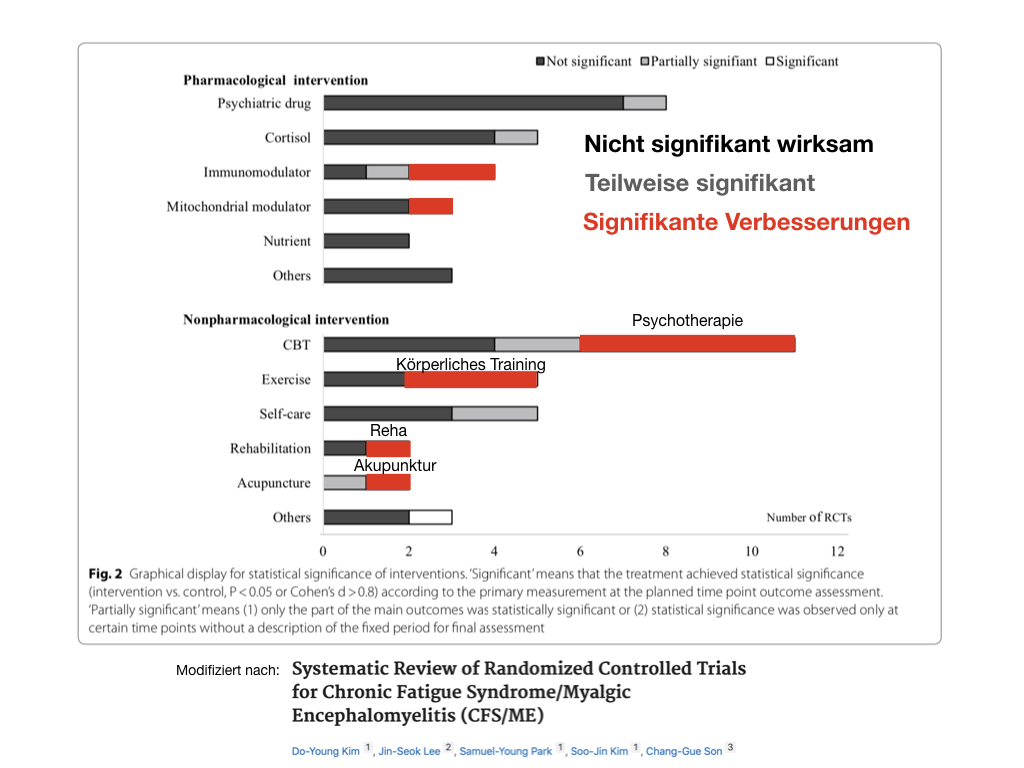
The main problem of therapy is that there are no clear treatment guidelines!
It is clear that simple drug treatments of the problem CFS are not effective. Hopes that there would be the "anti-CFS pill" have been thoroughly dashed.
Why? The reason - again similar to fibromyalgia - is that CFS involves complex regulatory disorders in the central nervous system. Thepages on fibromyalgia show part of this problem.
Regulatory disorder means that very far "up" in the hormonal system of bodily regulation (e.g. CRH) the entire vegetative system has become "misaligned". A multitude of hormones (thyroid hormone, growth hormone, prolactin, cortisone, vasopressin, etc.) no longer react as they originally did.
The result: a bewildering array of symptoms (freezing, sweating, sleep disturbances, water retention, gastrointestinal complaints, and, and, and).
Lowering of the swell
A second problem is the lowering of the stimulus threshold. The overstimulation by pain, gastrointestinal complaints as well as the often long-standing sleep disturbances lead to a general lowering of the threshold at which we perceive external stimuli.
Affected people develop an "input problem": signals from the environment increasingly reach them unfiltered and directly. The result: hypersensitivity to noise and light, sensitivity to touch, irritability and general emotional sensitivity. A "princess on the vine syndrome" develops over the course of months and years.
Much of the obvious advice, while correct, cannot be carried out by the sufferer.
Well-intentioned advice
What is clear is that if you should be affected, you should avoid doing anything to let the symptoms become chronic! The sooner you do something, the better! Only what? The advice, "do sports, get out of bed" may be correct in principle, but in most cases it will not be feasible, because the affected persons either have too little drive or too much pain.
Therapy principles
1. therapy must start slowly and take into account the individual's performance level.
It worsens the symptomatology to start a forced training that exceeds the patient's capabilities.
2. only by starting the therapy on many levels at the same time (multimodal therapy) there is a chance to act successfully on the complex disorder. Even proper therapies fail if they are used alone or sequentially.
For this reason, most outpatient therapies often have little success (this therapy for a while, then that), while inpatient treatments (different applications daily) have better chances.
3) It is important to restore the body's ability to regulate itself: the alternation of rest and activity, sleep and wakefulness, absorption and elimination, movement and rest, adaptation to cold and heat, light and darkness, etc.
I think it is important to raise the lowered threshold step by step and thus to limit the overstimulation.
5. important and often underestimated elements of therapy are, in addition to restfulsleep, agastrointestinal tract low in irritants and the absence ofedema, water accumulation in muscles and connective tissue.
6. psychotherapy is probably helpful if it is as targeted as possible: e.g. as cognitive behavioral therapy.
7. the earlier the therapy starts, the better. Sick leave alone does not improve the symptoms. Principle: As much rest as necessary, as much activity as possible.
Probably ineffective
Just at the beginning of the therapy of CFS some years ago, countless therapy approaches were tried. According to current scientific research, the following methods are not effective or have not been sufficiently proven:
- Immunoglobulins
- Interferon
- Antihistamines
- Aciclovir (drug against viruses)
- Fish oil
- Liver extracts
- Buspirone
- Somatotropin
- Fluoxetine (an antidepressant) e.g. Fluctin®, moclobemide, phenelzine
- Antirheumatic drugs (e.g. ibuprofen)
- MAO inhibitors (antidepressants)
- Melatonin
- Vitamins, minerals, trace elements
- probably: relaxation methods
Placebos?
Areview of the placebo effect revealed that it is surprisingly small in CFS (19.6%). "Contrary to conventional wisdom, the placebo response in CFS is low. Psychological-psychiatric interventions have been shown to have a lower placebo response, perhaps related to patient expectations."
Vitamins, minerals, trace elements and dietary supplements
The majority of all CFS patients we have seen take sometimes large amounts of vitamins, minerals or trace elements. The theory behind this: something is missing from the body.
But the success of this - sometimes costly - substitution is extremely limited. They probably do not go beyond a placebo effect. Above all, there is a lack of lasting and noticeable effects.
In areview, the studies published to date were examined with regard to the validity of substitution therapy. The sobering result: there is no rational basis for this form of therapy. The authors conclude, "Little evidence was found to support the hypothesis that vitamin and mineral deficiencies play a role in the pathophysiology of CFS and FMS and that the use of supplements is effective in these patients."
Similarly, dietary supplements do not deliver what they promise. Areview of 17 studies found that "This review found insufficient evidence to support the use of dietary supplements and elimination or modified diets for relief of CFS/ME symptoms. Studies were limited by the number of studies examining the interventions, small sample sizes, study duration, variety of instruments used, and studies that did not report on the method of dietary intake. Further research is warranted on homogeneous CFS/ME populations."
Help from Mother Nature
When scientific medicine does not help, hope often turns to natural remedies and alternative medicine. Even though the number of systematic studies here is small, the studies published so far are not very encouraging. Evidence of effectiveness of methods such as mind-body medicine, distant healing, massage, Tuina and Tai Chi, homeopathy, ginseng and nutritional supplements has not been provided.
Psychotherapy
Since no conspicuous physical findings can be found in CFS, many sufferers are recommended psychotherapy. This is rarely met with undivided approval by patients who feel predominantly physically impaired.
In our experience, psychotherapies alone are only marginally effective if they are not accompanied by other measures. This is also consistent with the literature(e.g.). Cognitive behavioral therapy has been best studied. This shows effects - however, these are not large.
For affected persons this can mean: It is right and good to start psychotherapy. This is especially true if unresolved conflicts in the present or past weigh on the soul. However, this alone is not sufficient. Other therapies must be used in addition in order to overcome the exhaustion permanently.
Training: very effective and very delicate!
Many patients with CFS suffer from depressive symptoms. It is often unclear whether this is a cause or a consequence of the symptoms of exhaustion. Regardless of this, antidepressants - often at low doses - can be helpful.
In thereview, the authors conclude, "Nonetheless, the data generated suggest that antidepressant medication is likely to be one of the right options for treating the core symptoms of CFS, regardless of whether comorbid depression is present."
Gold standard: multimodal therapy
As mentioned in the principles of therapy, there is not and probably never will be an "anti-CFS pill." What matters is a gradual restoration of regulation and adaptation. In a way, one could speak of "training". We rely on methods that are scientifically justifiable. In addition, we also set our own accents, especially with the circulatory training (seePOTS), the intensivebreathing therapy and the gradual physical activation.
Unfortunately, of all things, the main symptom stands in the way of this training. Due to the pronounced exhaustion, the sufferers often lack the strength to start anything at all, or even to seek treatment.
The solution in this case is to take small steps and start treatment as an inpatient, or - in our case - to live at the place of treatment, only a few steps away from the therapy measures. Training on a treadmill, where we can reduce the force of gravity, is very helpful.
Cold therapy in the whole-body cold chamber (-80°C) also has an activating effect without overloading.
If the symptoms have improved, further therapy steps can follow step by step and it is possible to switch to self-help to a large extent.
The treatment is basically related to the therapy of other functional disorders, especially to the therapy of fibromyalgia; both symptoms are possibly only different manifestations of the same disorder.
However, there are also differences. One seems to me not insignificant for the therapy: While with fibromyalgia great progress often occurs very quickly within 2 weeks of intensive therapy, with CFS one often needs a longer breath.
In particular the main symptom, the exhaustion does not say goodbye first. Only when sleep has deepened, pain has become bearable, gastrointestinal complaints and many other symptoms have disappeared, then the spirits of life are awakened again.
Or in other words: from my experience, exhaustion cannot be tackled primarily, directly, but via the "detour" of treating the extensive further disorders.
Therapy elements
Effective or helpful are:
- Circulatory training including cold therapy (cold chamber)
- Gradual build up of activity
- Respiratory therapy
- Measures to improve sleep
- Supportive psychotherapeutic procedures
- Acupuncture
- Some antidepressants
- Systematic self-help with self-help apps (online training
- Therapeutic procedures according to individual need
Online-App
Online therapy
Many patients with CFS and other fatigue syndromes are too weary for conventional therapy. Going to the doctor already is out of the question for you.
Rehab would be better, but there are hardly any specialized clinics here and little changes in three or four weeks. In addition, the usual rhythm of treatments is far too intensive for many sufferers. The result: the complaints often get worse instead of better.
We are currently working on online forms of treatment. In the process, we already have a very elaborate breathing app. We consider breathing to be a key element in the therapy of exhaustion.
Similarly, we have an app for therapy of POTS-type circulatory disorders.
Finally, relaxation and meditation exercises have been completed.
Research
In recent years, we have been able to establish that many exhausted patients exhibit changes in their breathing. These correlations are still very little researched, but allow the development of new therapeutic strategies.
We would therefore be very grateful if you would completethe following questionnaire.
You also have the possibility to leave an email at the end if you would like to be informed about the first results and where they will be published.
Thank you very much!
Videos: Case histories
Please keep the following in mind for all personal reports:
Please note