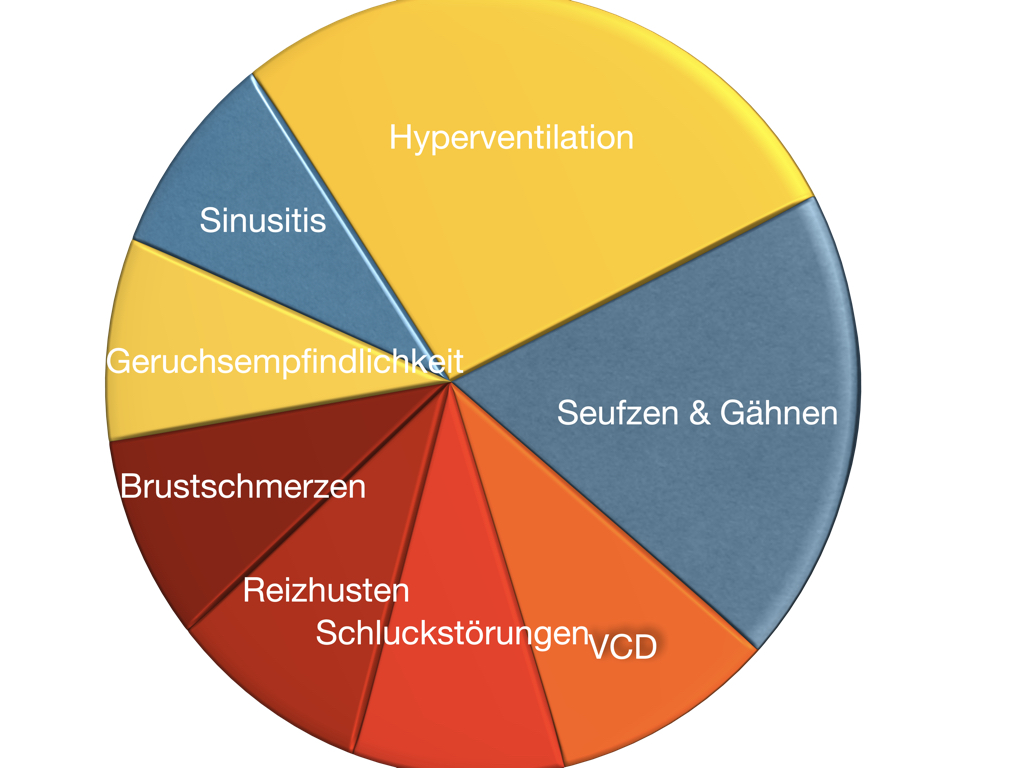
The symptoms differ considerably and yet there is a common cause: changes in breathing.
While the acute hyperventilation syndrome is a highly acute symptom (shortness of breath, anxiety, palpitations, dizziness, panic), the chronic hyperventilation syndrome is often overlooked. It usually manifests itself only indirectly and often only after years of symptoms. But the consequences for quality of life are sometimes much more serious and often lead to severe impairment, even retirement.
New:
Notice
Acute and chronic hyperventilation are part of functional respiratory disorders. Therefore, you can also find more information under the keyword "breathing disorder" on these pages.
Basics and introduction

Breathing plays an incomparable role in life. Without food we can survive for weeks, without drinking we can survive for days, but without breathing we literally run out of air after 3-4 minutes.
When we breathe, we take in oxygen and give off carbon dioxide. We speak of "combustion", and in fact every stove does nothing else: it burns a fuel with the help of oxygen and gives off carbon dioxide and water in return. What wood, coal or oil is to the stove, carbohydrates, protein and fat are to us.
The regulation of this process is finely regulated in our body. The oxygen concentration of the blood in healthy people under normal circumstances (no lung disease, no extreme altitudes) is almost 100% of the maximum possible value. The carbon dioxide content is about 40 mmHg (= mm mercury column).
How are you breathing right now?
If you are reading these lines right now, you are probably sitting quietly at your computer. You need energy; accordingly, you also need little oxygen and emit little carbon dioxide. In short, your breathing is calm and probably regular.
In such a case, your breathing rate will be around 12 to 15 puffs per minute. In children and adolescents, it is much faster. Depending on age, the resting rate here is 20-30 breaths.
But these normal values can be deceiving. Some people can lower their resting breathing rate to just a few breaths. 3-4 breaths per minute or less are possible when deeply relaxed.
It is different when you are exercising or running up stairs. Now you breathe rapidly to carry lots of oxygen through the blood to the muscles. The "exhaust gases", the carbon dioxide, they get rid of in the same breath - pretty handy!
Unconscious full automatic
Breath regulation is highly automated; we don't need to think about it. Even when we prepare for an action, we breathe a little faster and thus unconsciously adjust to the increased demand for oxygen.
This can be observed particularly well in athletes, e.g. weightlifters, who take a few deep breaths before the decisive attempt and then "get down to business". Sprinters behave similarly in the starting blocks, etc.
From a medical point of view, this makes sense, as the athletes have thus prepared themselves for the increased demand for oxygen and have already exhaled a little carbon dioxide as a prophylactic measure. It is a proven reflex that runs completely automatically.
As a result, we are not aware of our breathing. Even very conspicuous breathing (continuous mouth breathing, breathing that is too fast) usually remains hidden to those affected.
Classification
In the past, it was assumed that hyperventilation and dysfunctional breathing were synonymous. In fact, acute and chronic hyperventilation are the most common forms of so-called "dysfunctional breathing" even though exact figures are lacking.
Typical leading symptoms are shortness of breath, air hunger and shortness of breath without organic cause.
There are various attempts to classify them, andBoulding et. al. propose 5 types, which are briefly described here. In fact, the phenomena overlap. In particular, chronic hyperventilation is often found in the other forms of respiratory dysfunction.
But there is currently no "gold standard" regarding the classification. Other distinctions may also be useful.In fact, we see more or less pronounced changes in breathing in many, if not most, functional disorders.
Hyperventilation is described in detail below. A special form of hyperventilation occurs when the patient is sitting up from a lying position. It is called postural (= position-dependent) hyperventilation. It is usually accompanied by rapid heartbeat while standing, which is called postural tachycardia. For this purpose, acomprehensive presentation.
Frequent sighing and (often accompanying) yawning is a difficult phenomenon to describe. It can occur in addition to the normal occasional sighing up to incessantly (every minute) and can be an extremely agonizing condition. Sufferers suffer from constant breath retention and have the feeling of not being able to breathe properly.
Increased chest breathing
Increased chest breathing is found in physical diseases such as heart disease, COPD, diaphragmatic hypertension and also in very overweight people. However, it can also occur - frequently - as a purely functional (stress) symptom.
Reinforced abdominal press

Little known is the phenomenon of increased abdominal press. The air is actively expelled with force. In normal breathing, exhalation is a passive process. Only inhalation is actively performed. This increased abdominal press can occur in pulmonary disease is, however, also described as a functional disorder. We have seen patients who have developed veritable six-packs this way without exercise.
Paradoxical Breathing & Co.
Lack of synchronization of breathing is another disorder. Normally, the abdomen expands during inhalation and becomes flatter during exhalation. However, this can also be exactly the opposite and is then called "paradoxical breathing". In addition to this extreme form, there are other forms of lack of synchronization of breathing.
Normal breathing
Automatic
Breath regulation is highly automated, we don't need to think about it. Even when we prepare for an action, we breathe a little faster and thus unconsciously adjust to the increased demand for oxygen.
This can be observed particularly well in athletes, e.g. weightlifters, who take a few deep breaths before the decisive attempt and then "get down to business". Sprinters behave similarly in the starting blocks, etc.
From a medical point of view, this makes sense, as the athletes have thus prepared themselves for the increased demand for oxygen and have already exhaled a little carbon dioxide as a prophylactic measure. It is a proven reflex that runs completely automatically.
Central: Carbon dioxide
Most people assume that the oxygen content of the blood should be decisive for the respiratory drive. But this is not the case. As a rule, the production of carbon dioxide determines whether we breathe a lot or a little.
Another important factor is the acidity of the blood (pH). The more acidic the blood is (low pH) the faster breathing becomes. Breathing fast releases moreCO2, which causes the carbonic acid level in the blood to drop. Less carbonic acid means: the pH level goes back to the norm (pH 7.38-7.42).
The corresponding receptors for blood gases are located in the carotid artery (near the division point of the carotid artery) and in the aorta at the so-called aortic arch. There are also sensors in the brain stem. Right in its vicinity (medulla oblongata and pons) there is also the respiratory center, which controls respiratory activity.
Reflective control
But it is precisely this reflex that can also cause problems. It also occurs when we are mentally tense and do not move much afterwards.
If you are upset, angry or afraid about something, you often don't have the opportunity to run or physically attack your opponent afterwards. It would also be quite strange in many work situations to punch the air or pace back and forth in the office after an unpleasant phone call.
However, the age-old breathing reflex kicks in just as if we had to run from a tiger or attack an opponent. In short: we breathe too fast, which we are usually not aware of, because this rapid breathing is quite adequate to the inner tension.
The exhaust gas regulates the pH
Now an imbalance of the respiratory gases occurs. The oxygen concentration changes only insignificantly, since it is in the range of the theoretical maximum anyway.
The concentration of carbon dioxide is different. It drops and reaches 35 mm Hg and less, i.e. much lower than normal. One might object that it is only good to get rid of the unwanted gas. But it is not that simple.
Our body needs a basic concentration of this gas, otherwise the acid-base balance (pH) of the body changes. With too little carbon dioxide, the blood becomes too alkaline (= basic, the opposite of acidic). This has a variety of effects on other bodily functions.
Above all, the amount of freely available calcium in the blood decreases. Its concentration can thus decrease by up to 50%. Since calcium is essential for nerve and muscle activity, this is where the most severe changes are seen. Essentially, there is a general overexcitability of the nerves and a cramping of the muscles.
Acute hyperventilation
Highly acute and highly dramatic
In acute hyperventilation, the focus is primarily on abysmal fear. Those affected have the impression that they are on the verge of their own death. It is often a combination of fear of falling over, suffocation or a heart attack. At the same time, there is usually the feeling of being completely helpless.
The rapid breathing is usually not perceived. The feeling of shortness of breath and fear of suffocation dominates.
Symptoms often begin with tingling (formication) in the fingers, toes and mouth area. At the same time, numbness, tremors and muscle pain set in.
Later, cramps of the muscles occur. Usually this begins on the little fingers of both hands ("paw position"), later there is a tightening of the arms, stretching of the legs and cramping of the back muscles. In extreme cases, seizure-like conditions may occur - but usually not complete unconsciousness.
Usually, acute hyperventilation is accompanied by feelings of panic.
Electrolytes and circulatory disorders
The acute hyperventilation attack is also a dramatic event biologically. Respiration increases up to 500% of the norm. At the same time, the level of potassium, magnesium and calcium drops significantly. This leads to a general hyperexcitability of the nerves. Which complaints now appear depends on the individual "sore spot".
With the drop of the CO2 level, the cerebral blood flow is reduced at the same time. Head pressure or headaches are the result.
Dizziness, lightheadedness, "frosted glass," difficulty concentrating, headaches, irritability, sensitivity to the weather, sweating, freezing, cold hands and feet, urinary urgency, even premenstrual syndrome are exacerbated by lowered CO2 levels.
The pain in the left chest wall that occurs during hyperventilation is experienced by the affected person either as a stabbing pain or as a dull feeling of pressure behind the sternum or the left chest wall. In addition, increased palpitations occur.
This is most likely due to a so-called coronary spasm, a cramp-like narrowing of the coronary vessels.
Gastrointestinal complaints
Numerous gastrointestinal complaints can occur: Most notably, nausea, bloating, stomach discomfort, flatulence, increased bowel sounds, diarrhea, or other symptoms reminiscent of irritable bowel syndrome. Increased air swallowing (aerophagia) is also very likely.
Breathing symptoms
Chest tightness, lumpy or uncomfortable feeling in the throat, feeling of tightness, feeling like you can't breathe, yawning, sighing, irritable cough, and breathing too fast.
Psychological complaints
Inner restlessness and tension, fear of heart attack, fear of suffocation, fear of falling over, panic.
Chronic Hyperventilation
While acute hyperventilation syndrome is still relatively easy to recognize (subjective shortness of breath, increased breathing, severe anxiety, palpitations), this is much more difficult in chronic hyperventilation syndrome. Here, too, accelerated breathing is present, but it is only slightly intensified. The rapid breathing is practically undetectable from the outside, and the affected person does not perceive it either. The carbon dioxide level is only slightly reduced, and the acid-base balance is only slightly altered, since the kidney is able to have a balancing effect.
Many patients with chronic hyperventilation therefore know little or nothing about the problem. Nevertheless, in your case the CO2 level is already well below the norm in the relaxed resting state, namely 35 instead of 40 mmHg. There is evidence of a dependence of catecholamines (stress hormones) on the CO2 level, which again emphasizes the importance of breathing for various psychosomatic disorders.
Background chronic hyperventilation
The leading symptoms of chronic hyperventilation syndrome are:
- Dizziness and lightheadedness
- chest pain
- cold hands and feet
- fatigue
- listlessness
- drowsiness
- weather sensitivity
- Concentration problems
- Forgetfulness
- Irritability
- Tension, anxious or depressive symptoms.
Other complaints also occur, sometimes the whole variety of so-called functional disorders, whose common denominator is a lowering of the stimulus threshold.
pH shift
In chronic hyperventilation syndrome, the bicarbonate buffer of the blood is most likely borderline depleted so that even short-term accelerated breathing leads to a change in blood pH.
Such triggers can be anxiety, physical activity or even joyful excitement. For those affected, the connection is often not recognizable, since even a few breaths too many can trigger the symptomatology.
False choking alarm
The consequence: if theCO2 content of the blood rises to normal values, the body reacts as if suffocation were imminent. Shortness of breath, a feeling of constriction and even faster breathing with the typical consequences (acute hyperventilation) is the result.
This condition is also called "false suffocation alarm". Here is the truly groundbreaking work ofDonald F. Klein.
One of the typical signs: If theCO2 content of the air increases in a room because several people are staying there, this triggers the impression in the affected persons very early on: "This place urgently needs to be ventilated". They react hypersensitively to the increased carbon dioxide content of the air.
Irritable cough and exercise-induced asthma
TheCO2 level also has a pronounced effect on the bronchi. The higher theCO2 level, the more the bronchial muscles relax. Conversely, a decrease in carbon dioxide leads to constriction and spasm. At the same time, mucus formation is promoted.
As a result, free breathing is impeded, shortness of breath is the consequence, and this causes the affected person to breathe faster, which leads to a further lowering of theCO2 level. A vicious circle.
In bronchial asthma, some patients apparently suffer from a chronic hyperventilation syndrome with reduced carbon dioxide levels in the blood. Obviously, this subgroup also tends to suffer more frequently from anxiety and tension. The proportion of patients with asthma and lowered CO2 is likely to be substantial, although the numbers vary considerably in the literature.
Dizziness and lightheadedness
Very closely related to chronic hyperventilation is a special type of vertigo called staggering vertigo or phobic (anxiety) staggering vertigo.
There is a very unpleasant continuous vertigo in which, however, the affected person can stand effortlessly on one leg. Typically, no findings are found during examinations by the ENT physician or neurologist.
Chronic hyperventilation and the consequences
One of the triggers: near suffocation
Hyperventilation and fatigue
Very many patients with chronic hyperventilation feel peculiarly exhausted and at the same time internally restless. They have a feeling of drowsiness, inner restlessness or "absorbent cotton" in the brain.
Hyperventilation and panic
Panic attacks are very common during or after hyperventilation.
Frequency
Not rare!
Hyperventilation is not an uncommon symptom. There are estimates of 6-10% of all patients in an internal medicine practice. In anEnglish rural physician study, 10% of all patients were found to have an abnormal finding in theNijmegen questionnaire on hyperventilation.
Typically, physicians think that it is mainly women who are affected by the symptomatology. Surprisingly, however, both sexes have more or less the same tendency to accelerated breathing. However, it could be that more women find their way to the emergency room.
Very much more frequently obvious way patients with asthma bronchiale concerned. Here, every fourth person shows signs of hyperventilation.
In the course of life, the frequency of hyperventilation is supposed to decrease. But in fact we have seen a lot of people beyond retirement age who show significant hyperventilation. Often this is paired with chronic mouth breathing.
Often paired with panic
The frequency for panic attacks is given as 3-4% in the population. The highest frequency is in the age group of 20-30 years. Women are affected about twice as often as men.
If one summarizes all anxiety disorders, about 15% of all people suffer from them once in the course of their lives. At any given time, 7% are still affected by one of the various forms of anxiety disorder (panic attacks, agoraphobia, specific phobias, generalized anxiety disorder).
Diagnostics
Diagnostics
As a rule, acute hyperventilation is explained by the typical symptoms without further technical examination. During the physical examination by the physician, the lively reflexes (see above), which can go as far as convulsions, and the tremor are particularly noticeable.
If there is the possibility of a blood gas examination, a lowering of the carbon dioxide level and an alkalosis of the blood (blood becomes alkaline) can be found. This examination sometimes takes place, for example, at the pulmonary specialist. For this purpose, a little capillary blood (e.g. earlobe) must be taken. Disadvantage of the examination: It is a snapshot. If a patient has been sitting in the waiting room for a long time, the values may be completely normal. If, on the other hand, the patient is under stress or on an ergometer, other values would show up.
Nevertheless, the blood gas analysis is the "gold standard" for obtaining objective values.
Breathing gas analysis
Breathing gas analysis
During the breath gas analysis, theCO2 content of the exhaled air is checked. This is in balance with theCO2 level of the blood. This measurement is simple and can be done without blood sampling. Therefore, it can be used continuously both for diagnostics and for respiratory training.
The values are slightly (3-5 mmHg) below the value in the blood.
Blood gas analysis (BGA)
The standard procedure for determining a deviation of CO2, bicarbonate and pH is blood gas analysis. In this process, a drop of blood is obtained from the earlobe or fingertip and then immediately analyzed in a special device.
This test is performed, for example, by a lung doctor or in hospital emergency rooms.
Although these values are the most accurate, they represent only a snapshot. So it may be that after waiting calmly for the examination, the values are relatively normal. However, in the case of stress or physical strain, they are not.
We also perform this examination and put it in relation to the respiratory gas analysis.
Hyperventilation test
Often no doctor is available during a seizure. Affected people overcome the seizure on their own and do not see a doctor until later.
In such cases, a hyperventilation test can be performed subsequently. Under the protected environment of a doctor's office or clinic, the patient breathes approximately 60 breaths per minute for up to 3 minutes. During this time, the majority of symptoms should occur: Tingling, cramping, dizziness, visual disturbances, feelings of anxiety, lumpy feeling in the throat, palpitations and anxiety.
The test is more mentally than physically stressful, but should not be performed if you have bronchial asthma, severe heart disease or vascular disease. Please consult your physician before doing so.
Side effects: Headache, dizziness, lightheadedness, tingling - just the typical hyperventilation symptoms.
Quick help
We often perform the test with the following modification: Following the test, we let the patients breathe back. Within a short period of time, the symptomatology fades, providing a second proof of hyperventilation.
Small peculiarities: Not all changes result from changes in carbon dioxide and acid-base balance. The palpitations, tremors and anxiety are also due to the increased output of stress hormones and mental tension.
The stress hormones in particular take a while to dissipate. Thus, not all the symptoms may disappear with rebreathing, but only in the course of 30 minutes to 1½ hours, namely when the stress hormones (adrenaline, noradrenaline and cortisone) have also returned to the initial level.
Online test
You can take an online test (Nijmegen test) that gives you an immediate assessment of whether you are likely to have hyperventilation. It is the most widely used test in the scientific literature for diagnosing hyperventilation
Short term therapy
In therapy, it is useful to distinguish between acute measures and longer-term therapy.
A single hyperventilation attack/panic attack can usually be quickly brought under control, provided that the symptomatology is correctly recognized. With the right technique, it is usually possible to intercept the threatening symptomatology. This alone is already a great help for those affected.
However, a deep sense of insecurity often remains after such an experience. This then usually leads to further symptoms that are not so easy to treat. These include persistent dizziness, lightheadedness, jumpiness, anxiety, pressure on the chest, difficulty swallowing or other functional disorders.
In these cases, further measures are necessary. As a rule, we then carry out a multimodal therapy.
Obsolete methods
During a panic attack with hyperventilation, a vicious circle is triggered by an external event. Usually this happens in a tense situation; sometimes, however, it is trivial situations such as quickly sitting up or physical exertion.
Accelerated breathing causes a decrease in the carbon dioxide content of the blood, a pH shift and the consequent relative calcium deficiency of the blood.
In the past, therefore, attempts were made to neutralize the pH of the blood with a buffer infusion. Calcium was also given as an injection. Both methods are abandoned today. Injection of a diazepam-type sedative (e.g., "Valium®, Tavor®") is also considered obsolete today.
The therapy of choice in acute seizures is mental sedation and rebreathing.
Rebreathing
In rebreathing, you try to raise the carbon dioxide content of the blood again by inhaling your own used air. In this way, the carbon dioxide content of the blood slowly accumulates again.
A plastic bag of about one liter can be used for this purpose. This corresponds to the normal breath at rest. After 4-6 breaths, there should be a pause to renew the oxygen in the bag.
In itself, the technique is simple. Nevertheless, it is advisable to have it shown to you, e.g. by your family doctor.
Long term therapy
Breathing conversion
The acute hyperventilation attack usually requires only simple rebreathing. In the long term, the problem often lies in removing the fear of further attacks and treating possible triggering complaints and illnesses.
Often, after one or more hyperventilation attacks or panic attacks, there is a constant fear of further such states experienced as life-threatening. Of all things, this fear leads - unconsciously - to accelerated breathing. Other symptoms such as dizziness, lightheadedness, inner restlessness and vegetative symptoms are often added and intensify the complaints.
The body adjusts to this permanent tension. Presumably, this leads to a permanent adjustment of the target value forCO2 in the brain stem. This means that those affected have the impression that they are breathing completely normally, but in fact this is always a little too fast.
Little misunderstanding: hyperventilating as "therapy
Change of the "set point
One essential goal is to raise the target value for theCO2 content of the blood. There are various techniques for this, but they have one thing in common: IncreasedCO2 levels are coupled with relaxation and freedom from anxiety.
Calm, relaxed breathing is one of the royal roads to inner balance. We therefore use a range of breathing therapy techniques that can then be continued at home.
A special feature is a breathing therapy in which the carbon dioxide level is measured directly. With this biofeedback method, a device immediately indicates learning success.
Other biofeedback methods combine breathing with sounds. A device measures how fast the breath is and translates this into music. The calmer the breath, the more pleasant the music. Over the course of a few minutes, the accelerated breathing calms down.
In the end, patients often manage effortlessly with just a few breaths per minute.
Confidence and trust
The permanently accelerated breathing very often leads to a state of inner agitation and deep insecurity. In a further step of the therapy, therefore, an attempt is made to restore security and well-being.
Conversations are used for this purpose, in which an understanding of the symptomatology and its origins is gained. But beyond that, it is about the sensual experience that the body feels good and vital again. Massages, physiotherapy, exercise convey confidence and trust.
In our view, this part of the therapy plays a major role in achieving quick success.
Regaining autonomy
Those who have been unsettled by unexplained discomfort for a long time often withdraw strongly. Many sufferers no longer dare to go to the places where they experienced a panic attack or hyperventilation. Some then feel safe exclusively at home and only leave the house when accompanied.
But what reduces anxiety in the short term makes it worse in the long term. Therefore, regaining lost self-confidence and autonomous activity is another important step in therapy.
Multimodal therapy
Hyperventilation and panic attacks rarely occur as isolated symptoms. Most often they are coupled with other vegetative and functional complaints. Very common is persistent vertigo symptomatology. Irritable stomach, irritable bowel complaints, sleep disturbances, sensitivity to cold and blood sugar fluctuations are also often associated with the symptomatology.
For those affected, the multitude of symptoms is often confusing and disturbing. In fact, there is a common cause behind them, as illustrated elsewhere.
We therefore usually treat not only breathing, but comprehensively with a multimodal therapy to address body, mind and spirit simultaneously.
Central: Capnometer-assisted breathing training
In functional respiratory disorders, the blood carbon dioxide is usually too low. This is especially true during stress and internal tension. The problem: You cannot perceive the carbon dioxide content of your blood. It is similar to blood pressure. Even people who have had elevated blood pressure for years or decades notice little or nothing of it.
Therefore, measuring the CO2 level with a so-called capnometer (kapnos = smoke) is of central importance to us. We use such devices not only diagnostically but also therapeutically. Above all, devices that determine the CO2 content of the air we breathe have proven their worth. This corresponds to the CO2 of the blood.
If you now measure the CO2 content of the air during breathing exercises, you can see whether you are performing the exercises correctly. It is unfortunately the case that many breathing exercises, although technically correct, nevertheless lead to a highly undesirable reduction in CO2 levels.
Duration
Our experience shows that only close-meshed and intensive treatments achieve good results. We therefore usually carry out an intensive therapy lasting 1-3 weeks, during which a wide range of individual measures are applied.
This usually leads to a significant improvement of the symptoms. This means that the symptoms have not yet completely disappeared, but can still be felt, especially in stressful situations. But the patients have acquired techniques with which they can control their complaints themselves.
This knowledge is the decisive step in overcoming helplessness and regaining a normal life for themselves.
We often supplement this on-site therapy with guided online self-help supported by an app.
Breath app
Over several years, we have been able to develop an app that you can use to train at home. This is suitable as a supplement to the above measures or as a stand-alone therapy in less pronounced cases.
Videos
Please follow the instructions that apply to all personal reports.
Important note